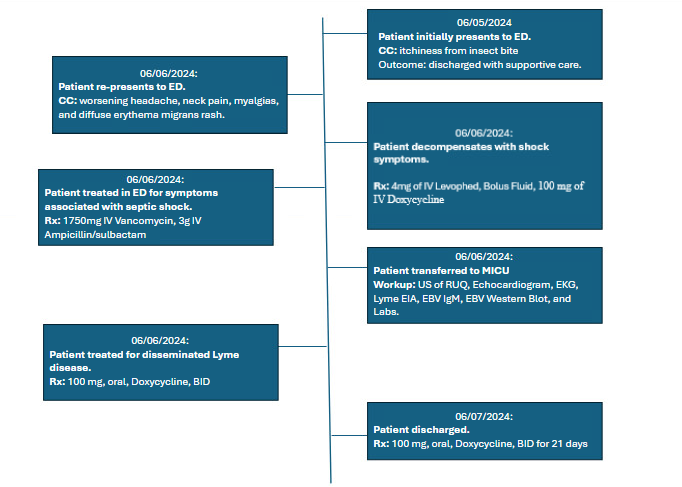
Case Presentation: The day before his wedding, a 22-year-old male presented to the emergency department with one week of worsening joint pain, myalgias, headache, and rash. Symptoms began weeks after visiting a park in Michigan and several days after walking in tall grass during his bachelor party in Iowa. He presented to the emergency department febrile, tachycardic, and hypotensive. Physical examination was notable for erythema migrans. Laboratory analysis revealed an elevated CRP, procalcitonin, sedimentation rate, LFTs, troponin, and leukocytosis. Lyme antibody test was positive. EKG findings showed T-wave inversions in the anterolateral leads, a prolonged PR interval without AV block, and sinus tachycardia. Doxycycline was initiated, however, the patient rapidly decompensated, requiring vasopressor support. Subsequently, antibiotic therapy was escalated to ampicillin/sulbactam and vancomycin to broaden coverage and for concerns for anaphylactic reaction, which was later ruled out by a normal tryptase level. Cardiac workup was negative, including an echocardiogram. With clinical improvement, therapy was deescalated to doxycycline monotherapy. He was discharged with 21 days of Doxycycline. Follow-up Lyme Ab testing (western blot) was consistent with an acute infection.
Discussion: It is exceedingly rare for Lyme disease (LD) to present with shock. The most common cause is cardiogenic shock, occurring in less than 5% of cases with cardiac manifestations.1 Our patient had no evidence of significant cardiac dysfunction from Lyme carditis. Another possible explanation for shock in LD is co-infection with Borreli, Anaplasma, Babesia or Ehrlichiosis. While co-infection is possible, it is rare and no evidence of coinfection was found in this case.2,3 While there was initially concern for anaphylactic shock, this was ultimately ruled out and the patient was discharged on doxycycline therapy. A final possibility would include Jarisch-Herxheimer reaction (JHR), which has been associated with LD in rare cases.4 However, JHR usually presents hours after treatment initiation. Given the very rapid deterioration after the initiation of doxycycline, developing shock secondary to LD is most likely. 5
Conclusions: It is exceedingly rare for Lyme disease (LD) to present with shock, which is most commonly due to secondary bacterial infection in the setting of chronic treatment (which was not present in this case). Patients with suspected LD presenting with shock should have all other etiologies ruled out. In this case, no other etiology provides a satisfactory answer to the patient’s hypotension requiring the initiation of vasopressors and we suspect this was most likely due to acute LD.