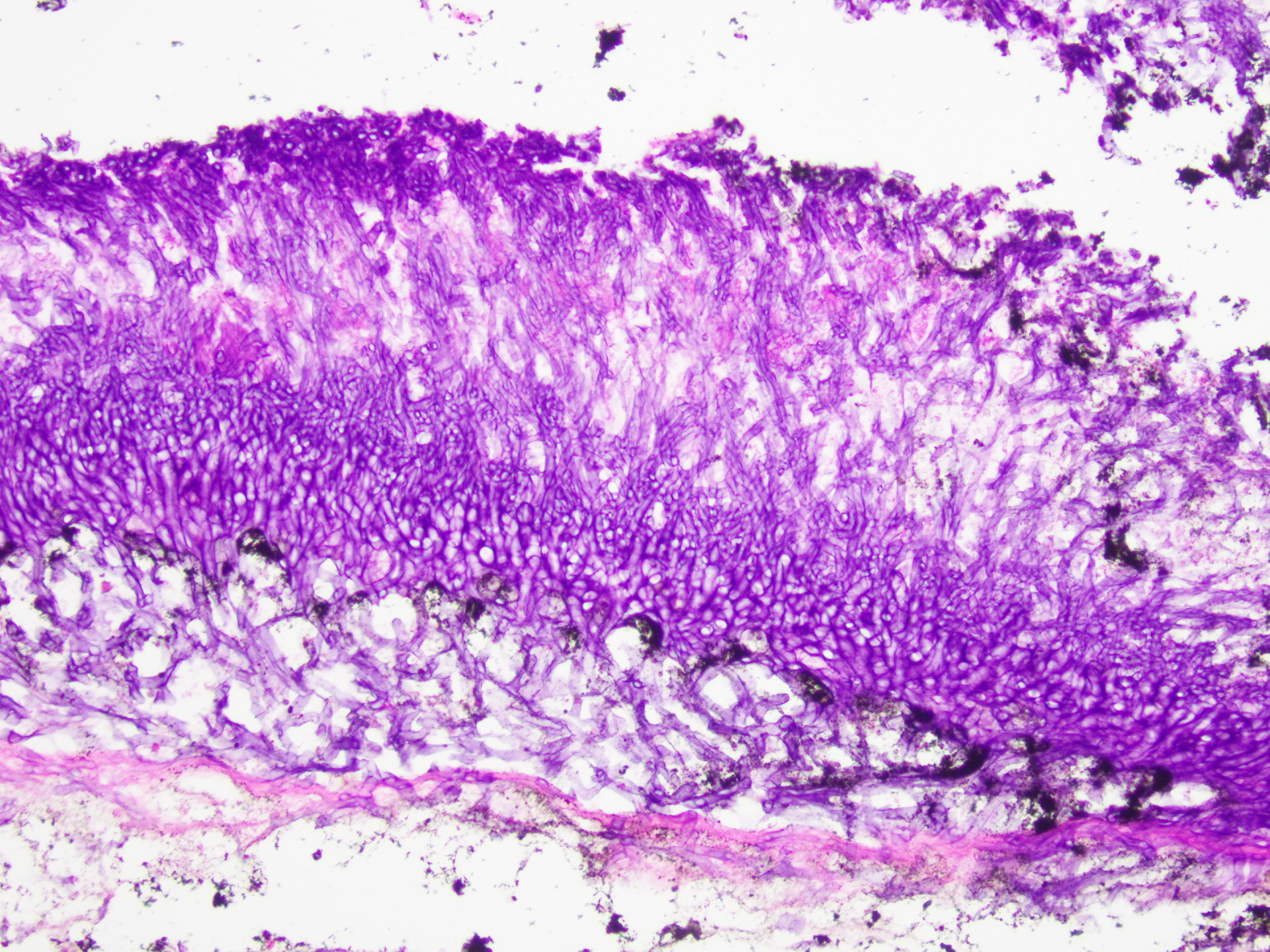
Case Presentation: Reports of COVID-19 Associated Pulmonary Aspergillosis (CAPA) have increased. Most cases are in persons older than 65 years of age, who are mechanically ventilated, have chronic lung disease, and/or are immunocompromised. Aspergillus can lead to infections such as chronic pulmonary aspergillosis, allergic bronchopulmonary aspergillosis, and invasive pulmonary aspergillosis (IPA). IPA has the highest mortality rate even when treated with appropriate antifungal therapy.This is a unique case of IPA in a 40-year-old Hispanic man with minimal risk factors who received guideline-directed anti-fungal treatment. His medical history was significant for uncontrolled insulin-dependent type 2 diabetes and tobacco use. He had been hospitalized 3 weeks prior to presentation for DKA and COVID-19 pneumonia (PNA) requiring ventilatory support, steroids, and monoclonal antibody therapy. His exam was remarkable for sinus tachycardia with diminished breath sounds over the left upper lobe and was otherwise normal. Labs were notable for leukocytosis (32K), anemia, hyponatremia, elevated procalcitonin, and hyperglycemia. Chest X-ray showed a lingular consolidation with post-obstructive atelectasis. CTA chest showed patchy peripheral ground glass opacities and a tree-in-bud pattern in the left upper lobe. He was started on broad spectrum antibiotics for a superimposed health-care related PNA and steroids for left sided pleuritic chest pain. He underwent bronchoscopy with biopsy which noted mucinous-appearing polypoid masses firmly adherent to the bronchial wall in the left upper and middle lobe bronchus. Histology revealed numerous fungal septate hyphae with acute angle branching forming a mycetoma (“fungus ball”) with background inflammation and necrotic respiratory mucosa. He was diagnosed with an aspergilloma with signs of necrotizing PNA. HIV and QuantiFERON testing were negative; the fungitell assay was positive. Oral voriconazole for antigen positive aspergillus and Augmentin for bacterial PNA were started. At this point, the patient was considered stable and discharged home with outpatient follow up. Unfortunately, the patient returned to the hospital one week later for worsening cough, congestion, and diarrhea. He was started on broad spectrum antibiotics for PNA and continued voriconazole for his invasive mycetoma. He tested positive for Clostridioides difficile and was treated with oral vancomycin. Throughout his hospitalization, he continued to have fevers, leukocytosis, and down-trending hemoglobin, despite multiple transfusions and no evident source of bleeding. His course was complicated by acute pulmonary hemorrhage from mycetoma rupture leading to cardiac arrest and eventual death.
Discussion: While CAPA incidence has increased in post-COVID immunocompetent patients, it is uncommon to rapidly develop IPA with necrotizing PNA. Furthermore, acute pulmonary hemorrhage associated with mycetoma is rare. Physicians are encouraged to administer aggressive antifungal therapy with possible resection in such patients to decrease the already high mortality rates associated with IPA. Given the rapid decline, despite guideline directed therapy, this case questions the possibility of increasing voriconazole-resistant CAPA cases as a leading cause to this patient’s worsening necrotizing PNA, pulmonary hemorrhage, and eventual death.
Conclusions: This unique case highlights the complexities associated with COVID-19 infection.