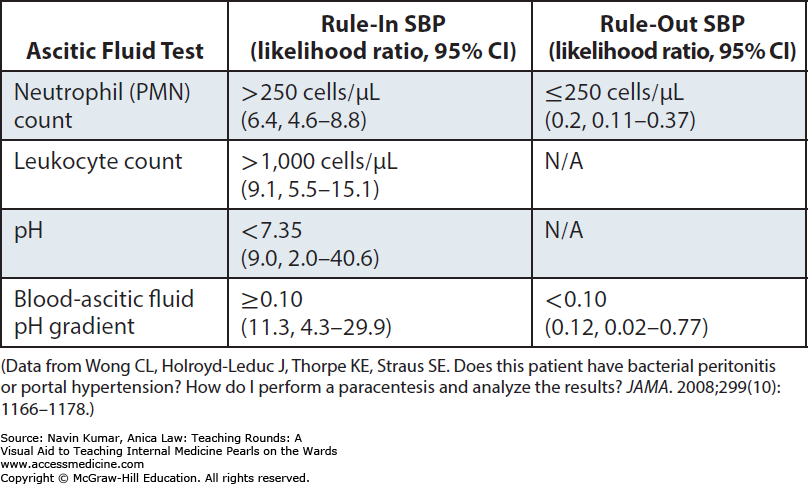
Case Presentation: 48-year-old female with past medical history of cirrhosis secondary to HBV (on entecavir) and EtOH, decompensated by hepatic encephalopathy and ascites, coronary artery disease s/p stenting to LAD in 2009 presented to the hospital with abdominal pain and distension for a 1-week duration. She stated that the pain radiated to her back and had been getting progressively worse over the past week. She additionally admitted to myalgias, nausea and vaginal discharge for the past few days. On arrival patient was hemodynamically stable and afebrile. CBC demonstrated WBC 19.8 and lactate of 3.6. CT abdomen demonstrated thrombosis involving the superior mesenteric vein, splenic vein, and main portal vein with a cirrhotic liver with extensive gastric and paraesophageal varices, large ascites and splenomegaly. Paracentesis was performed and notable for 1,180 WBC and 89% PMNs. Patient was started on IV ceftriaxone for spontaneous bacterial peritonitis. Pelvic exam was without any signs of PID, however, NAAT of vaginal probe was positive for Neisseria Gonorrhea. Initial gram stain of peritoneal fluid demonstrated gram negative cocci with final culture results speciating to Neisseria Gonorrhea. Patient was treated with high dose Ceftriaxone for 7 days with resolution of SBP with repeat therapeutic paracentesis 5 days following of initiation of therapy without evidence of infection.
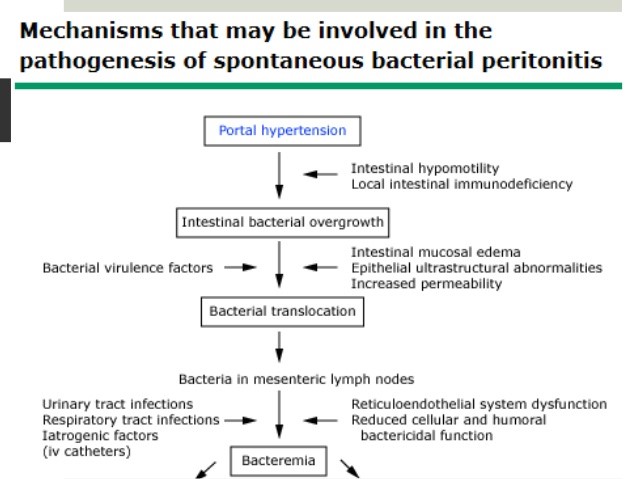
Discussion: Spontaneous Bacterial Peritonitis is an ascitic fluid infection without an obvious intra-abdominal surgically treatable source. An infection often seen in cirrhotic patients, SBP is associated with significant increase in mortality. In-hospital mortality for the first episode ranges from 10-50% and one-year mortality after a first episode of SBP has been reported to be between 31 and 93%. In the majority of patients, translocation of enteric organisms into the peritoneum is the suspected path of entry for patients found to have SBP. However, in this patient with an asymptomatic gonorrhea infection, the likely route was transfallopian migration of the organism from the cervix. There has been 1 case report in 1985 describing a similar case in which it was hypothesized that this was indeed the most likely route of migration given a lack of systemic symptoms such as arthritis, meningitis, tenosynovitis effectively decreasing the probability of systemic infection and without CT evidence of underlying abscess.
Conclusions: Given our patient’s asymptomatic gonococcal infection of the cervix and of the ascitic fluid, it is most likely that transfallopian migration was the most probable route of entry. Other conditions commonly discussed, such as Fitz-Hugh-Curtis syndrome, likely have similar pathophysiologic mechanisms.