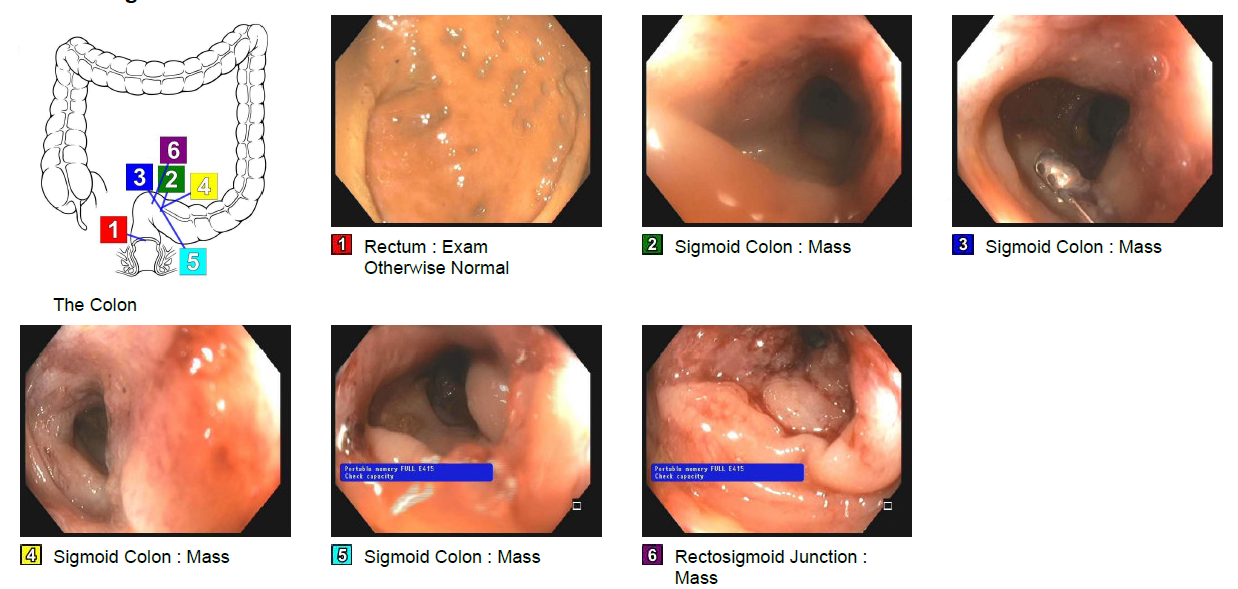
Case Presentation: 60 year old female who presented with generalized abdominal pain and distension. Associated featured included unintentional weight loss of 20 lbs, fatigue, nausea, vomiting. She denied melena, hematochezia, diarrhea or pelvic bleeding. Her past medical history was significant for Estrogen Receptor (ER) positive, Progesterone Receptor (PR) positive, human epidermal factor 2 (HER2) negative, stage 1 right breast lobular cancer for which she underwent bilateral mastectomy the same year. The left breast was removed pre-emptively and she took Tamoxifen for five years.Physical exam revealed stable vital signs, distended abdomen, generalized tenderness with positive fluid thrill.Initial CT scan of the abdomen and pelvis showed a moderate sized right sided pleural effusion, large ascites in the abdomen, an enlarged uterus with multiple fibroids with fluid filling the endometrium with enhancement. She underwent thoracentesis and paracentesis which were consistent with an exudative process suspicious for malignancy versus tuberculosis (TB); workup for both of these was negative. Elevated tumor markers CEA, CA 27-29, CA15-3 and CA125 were noted. Her CBC was remarkable for normocytic anemia.Later, she was evaluated by the gynecological oncology team due to the concern for a primary uterine malignancy.Subsequently MRI abdomen/ pelvis was done to evaluate for her primary malignancy, this revealed distal descending colon narrowing concerning for a colonic mass along with peritoneal carcinomatosis. No endometrial mass was noted.Subsequently, the patient underwent flexible sigmoidoscopy which showed an infiltrating, circumferential partially obstructing mass in the rectosigmoid colon. Biopsy results were consistent with invasive lobular cancer with a primary breast cancer.The patient was also evaluated by gastroenterology for any possible intervention with diverting colostomy or stenting for her colonic mass but given her metastatic disease and higher risk versus benefit of surgery, conservative management was recommended.The teams discussed the the non-curable nature of disease with the family. The patient was subsequently started on letrozole and abemciclib and discharged to skilled nursing facility with scheduled frequent paracentesis.
Discussion: The most frequent sites of metastasis from breast cancer include liver, lung, brain and bones. Involvement of GI tract secondary to a primary breast malignancy is rare and the most common histopathological diagnosis is Invasive lobular carcinoma. The mechanism of cancer dissemination is thought to be primarily hematogenous; others include lymphatic and peritoneal.Since the spectrum of clinical presentation of metastatic breast cancer to colon is very wide and maybe non-specific, this poses a significant diagnostic challenge.The prognosis of metastatic breast cancer to gastrointestinal tract is dismal with very few patients surviving beyond 2 years. As per statistics from National Institute of Health, in 2015, 71.6% women had a screening mammogram while 63.4% of women got colonoscopy within the screening age group indicating that while women are getting the mammogram, there still exists an 8.2% difference between the colonoscopy and mammogram rate.
Conclusions: This case demonstrates the importance of considering metastatic breast cancer as a differential when a patient presents with non-specific abdominal complaints in the context of a previously treated primary breast malignancy.