Background: Chronic obstructive pulmonary disease (COPD) is a leading cause of hospital readmissions, with national 30-day readmission rates reaching as high as 22.6% [1]. These readmissions place a significant financial burden on healthcare systems, with one study showing that the cost of a COPD readmission can exceed that of the initial admission by 18% [2]. At our hospital, the COPD readmission rate was recorded at 35% in 2023, underscoring the need for targeted interventions to address this issue. The high readmission rate can be attributed to several factors, including insufficient awareness of the progressive nature of COPD, lack of standardized care protocols, and gaps in the care transition process. These challenges present an opportunity to enhance the quality of care for COPD patients and reduce the frequency of avoidable readmissions.
Purpose: To address these issues, we implemented a multi-disciplinary, collaborative initiative designed to improve care transitions and reduce COPD readmissions. Our approach emphasized early patient education, comprehensive provider handoffs, timely involvement of pulmonary and palliative care teams, and systematic care transitions.
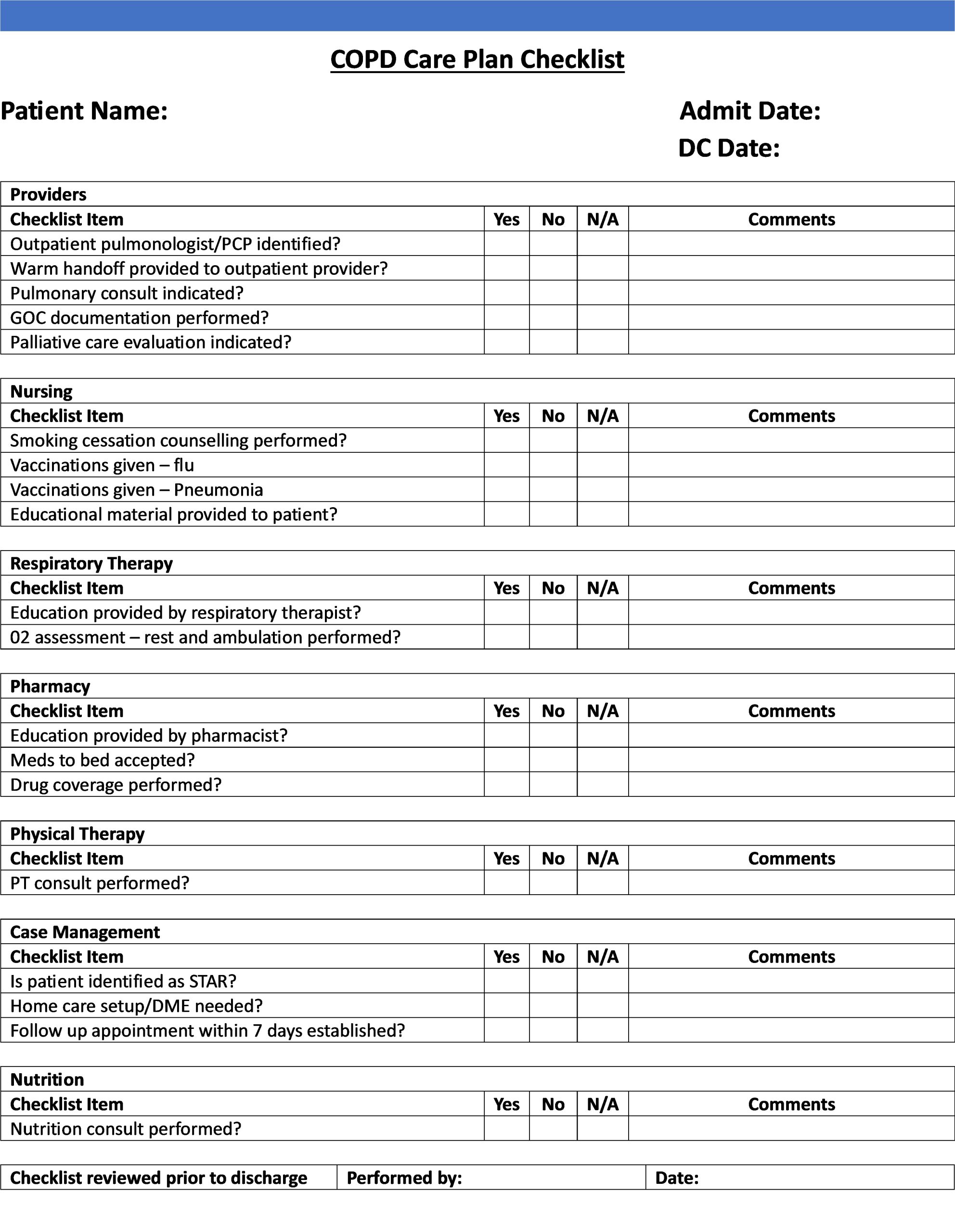
Description: A committee of key stakeholders—including hospitalists, respiratory therapists, physical therapists, pharmacists, nurses, nutritionists, case managers, pulmonologists, and palliative care specialists—was formed to identify gaps in care and develop strategies to address them. Over several months, the committee conducted focused discussions and created a checklist of essential tasks to be addressed during hospitalization, streamlining the care process.Hospitalists led efforts to ensure proper diagnosis and documentation, prioritized early consultations with pulmonary and palliative care teams, and facilitated goal-of-care discussions with patients during the index admission. Additionally, they ensured warm handoffs to community providers upon discharge. Respiratory therapists provided patient education on inhalation devices and home oxygen needs, while pharmacists conducted medication counseling, verified drug coverage, and implemented “meds to beds” programs to promote adherence. Physical therapists introduced early mobilization strategies, and nursing staff provided vaccinations and smoking cessation counseling. Nutritionists addressed dietary needs, and case managers coordinated home equipment needs and follow-up appointments with primary care providers or pulmonologists within seven days of discharge.Once a patient with a COPD exacerbation was identified, the multi-disciplinary team was notified, triggering each discipline to take ownership of implementing the checklist items relevant to their scope of practice. We monitored these patients for 30 days post-discharge to evaluate readmission events, focusing on both avoidable and unavoidable causes.
Conclusions: This initiative has raised awareness among team members about the critical role of coordinated care in improving outcomes for COPD patients. With hospitalists leading the effort and with the support of all key disciplines, we believe we have significantly improved the quality of care for COPD patients at our hospital. Although our checklist implementation is still in its early stages, we believe a multi-disciplinary approach is key to success in reducing COPD readmissions and improving patient outcomes in the long term.