Background: Rapid recognition of deteriorating patients and efficient physician – nursing communication is essential for patient safety and improved health outcomes (1,2). We conducted a pilot study at a tertiary care academic hospital in September, 2024 with intervention to improve communication between night physicians (nocturnists) and nurses (RN).
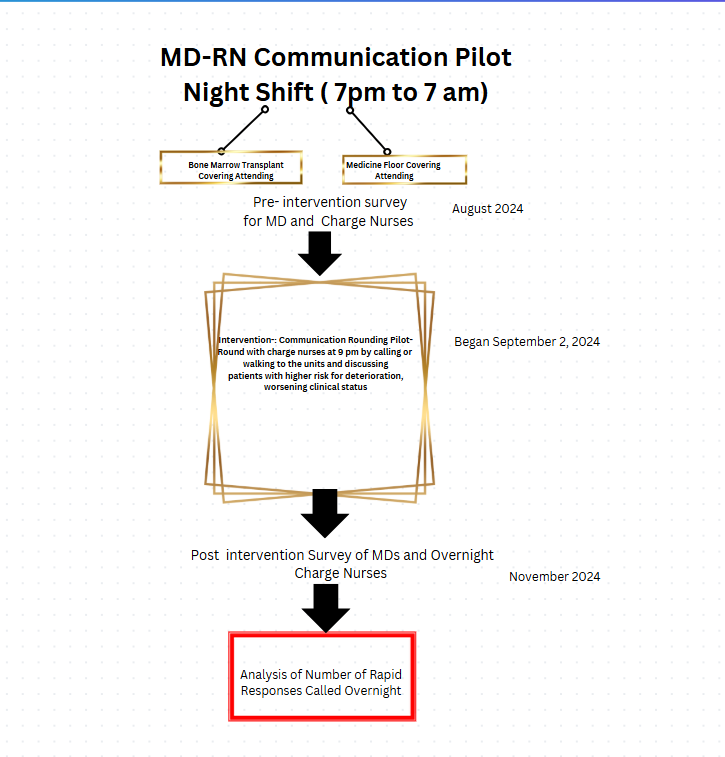
Methods: At the study site, night shifts last from 7pm-7am with two nocturnists covering Hospital Medicine and Bone Marrow Transplant service patients. Intervention included nocturnists either calling the charge nurses over telephone or conducting “walk rounds” on different units. During the rounds, patients with risk of deterioration (worsening respiratory status, sepsis alerts, stroke-like symptoms, etc.) were identified. Any outstanding orders- such as labs, expiring medications and telemetry were also discussed. These rounds were performed at around 9 pm.Pre intervention, we performed a survey for nocturnists and nurses to assess their attitudes and practices regarding communication quality. Basic demographics and free standing comments were collected. Following the implementation of the pilot for a month, a post survey was performed amongst the same participants to assess any change in attitudes and practices regarding communication . The number of rapid responses before and after the pilot study were analyzed as an objective measure. Descriptive analyses were performed to measure the outcomes. (See Figure 1).
Results: Preintervention survey response was RN (n=74), nocturnists (n=13); 53% of RN had > 8 years experience while 46% nocturnists had 1-4 years experience. In Presurvey, 53% (7/13) of nocturnists were dissatisfied with existing communication. Some of the challenges included delayed response times and inability to identify the covering nurse. About half noted they had a moderate amount of awareness of unstable patients. Over 90% felt communication with Emergency Department (ED) RN needed improvement. Two thirds of RN felt the response time of physicians should be improved, while 58% identified difficulty in knowing the covering physician.Post intervention survey had response rate: RN (n=38) and nocturnists (n=13). On the post-intervention survey, 90% of physicians felt the pilot was helpful in improving communication. However, 61% felt the pilot was too time-consuming. Post- intervention, 70% of nurses were satisfied with communication with physicians. Almost all of RNs (94%) did not feel the intervention rounding was time-consuming and 97% felt the pilot should be continued. Overall, charge nurses expressed better support knowing who the covering physicians were. Preintervention, there were 41 rapid responses (RRT), while 22 during the pilot intervention month. RRT increased to 43 in post intervention month. (See Figure 2).
Conclusions: In our intervention pilot study to enhance communication, we noted mixed results. While nocturnists felt the intervention was helpful initially, their participation dropped due to perception of being time consuming. Rapid response event rate was reduced by 46% in the intervention month though returned to preintervention level in the subsequent month. This may be a result of secular trends but likely affected by reduced nocturnist participation. Future interventions will include overnight code RN and ED inpatient nurses as stakeholders. This pilot highlights the small measures hospitalists may implement to improve communication with nursing and to help identify declining patients earlier.