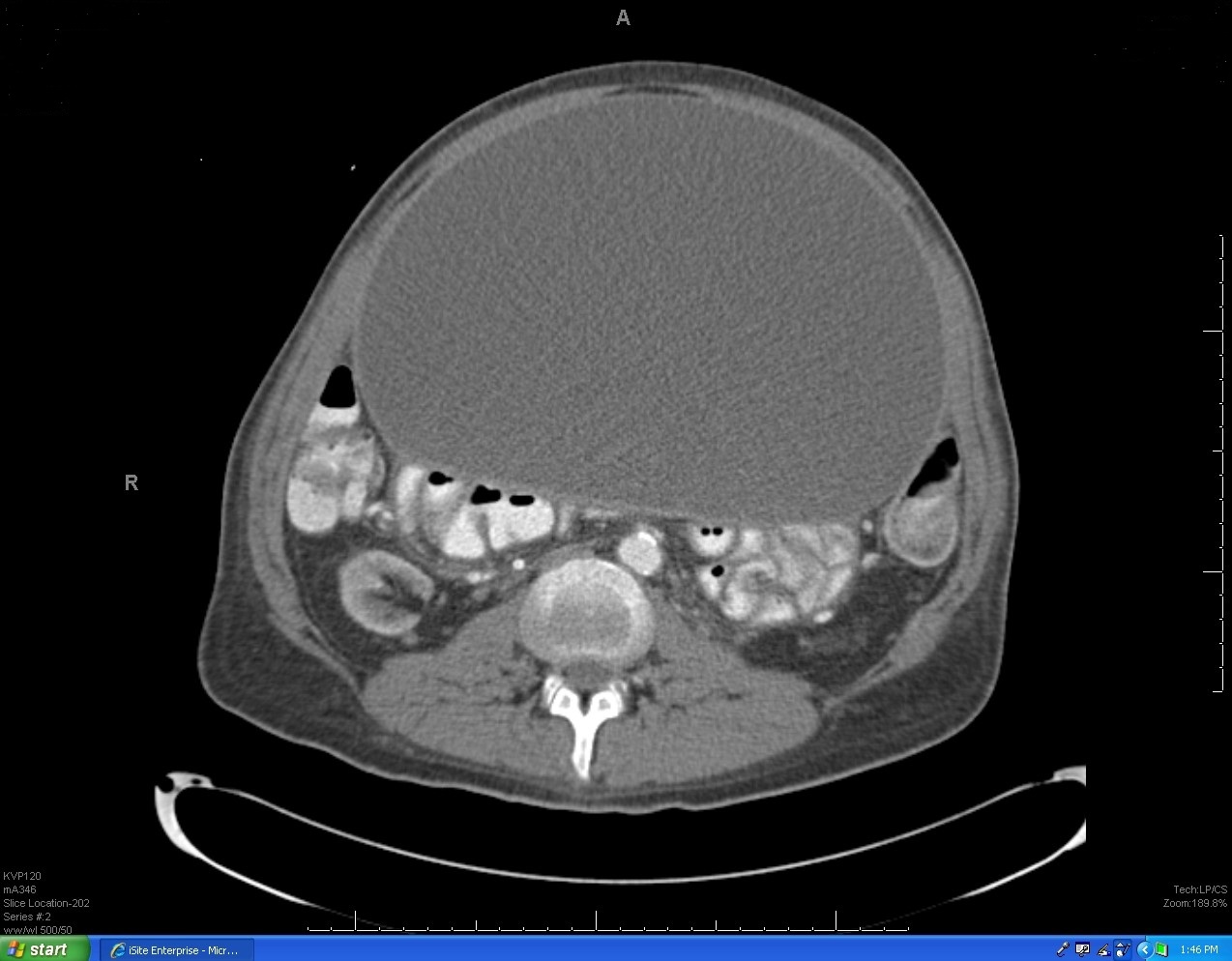
Case Presentation: A 43-year-old man with end-stage renal disease (ESRD) presented with six months of progressively worsening abdominal distention, diffuse abdominal pain, early satiety, and unintentional thirty-pound weight loss. He previously had undergone peritoneal dialysis for four years, complicated by multiple episodes of peritonitis and removal and replacement of multiple peritoneal dialysis catheters. Six months ago, peritoneal dialysis was discontinued and hemodialysis was started. Abdominopelvic computed tomographic (CT) scan revealed a large (24 x 17 x 22 cm), loculated fluid collection in the anterior portion of the abdomen, extending inferiorly into the upper false pelvis (see attached CT image). Adjacent bowel loops were markedly compressed and displaced, but without bowel obstruction.Ultrasound-guided drainage of the cystic lesion produced nearly five liters of bloody fluid and improvement of the patient’s symptoms. Cytology revealed cystic debris and blood, without malignant cells. Microbiologic analysis of the fluid revealed no evidence of infection. Four months later, the patient presented again, complaining of abdominal pain, nausea, and vomiting. Repeat abdominopelvic CT scan revealed recurrence of the intra-abdominal fluid collection and possible bowel obstruction. Exploratory laparotomy revealed a large peritoneal cyst, densely adherent to adjacent small bowel and the anterior abdominal wall. Approximately 1800 mL of thin, brown, feculent-smelling fluid was drained. There was evidence of small bowel perforation at the attachment site of the cystic structure. Cyst resection and ileocecectomy, with ileocolic anastomosis, were performed. Lab analysis of the cyst fluid revealed bloody debris, without malignancy or infection. Pathology of the cystic structure revealed encapsulated organizing hematoma. Repeat abdominopelvic CT scan performed three months after surgery revealed no evidence of recurrent peritoneal cyst.
Discussion: An intraperitoneal inflammatory pseudocyst encasing an in situ peritoneal dialysis catheter is a very uncommon complication of peritonitis in peritoneal dialysis, with few case reports. Rarer still is development of a peritoneal pseudocyst following peritoneal dialysis catheter removal, as occurred in this patient. In this patient’s case, it is postulated that the combination of prior peritoneal dialysis and frequent episodes of peritonitis produced a chronic intraperitoneal inflammatory state. The resultant distortion of normal peritoneal absorptive function likely allowed for the development and persistence of a peritoneal pseudocyst. Bowel perforation was the result of chronic intra-abdominal fibroadhesive disease, complicated by ischemic necrosis of bowel.
Conclusions: Patients with ESRD are frequently encountered by hospitalists. Assessment for and management of the multiple possible complications of current or prior dialysis is an essential part of our practice. The presence of a peritoneal pseudocyst, although rare, should be considered in the differential diagnosis of progressive abdominal distention if a patient has a history of prior peritoneal dialysis.