Background:
On July 1, 2007, the CMS launched the Physicians Quality Reporting Initiative (PQRI) as a voluntary pay‐for‐reporting program to reward individual physicians for providing quality care based on 74 performance measures. The program calls for a bonus of up to 1.5% of total allowed charges for the Medicare physician fee schedule with claims‐based reporting using CPT category II codes.
Purpose:
The purpose of this innovation was to improve hospitalist performance by grouping PQRI performance measures into bundles that harmonize with hospitalist work flow. PQRI reporting requires identifying eligible patients, providing appropriate documentation in the medical record to fulfill the measure requirement and then capturing for claims submission the CPT category II and evaluation and management codes associated with measure numerators and denominators. Bundling of measures to time of admission and discharge clarifies when a given measure should be considered and who is responsible for implementation, thereby avoiding ambiguity when multiple physicians are involved in a patient's care
Description:
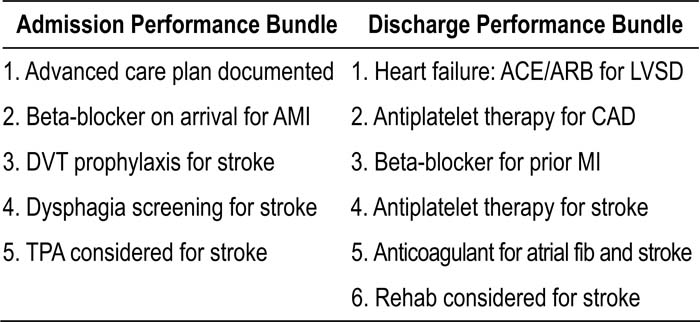
Eleven of the 74 PQRI performance measures were identified as relevant for performance reporting by hospitalists based on measure specifications that allow for inpatient reporting. The measures were categorized for implementation at the time of hospital admission or discharge. Eligible patients then receive care that fulfills the measure requirement on admission or discharge, with documentation that fulfills the measure requirement completed in the history and physical or discharge summary. The claims‐based performance reporting is attached to the admission or discharge billing codes submitted to Medicare. The admission and discharge performance measure bundles are listed in Table 1.
Conclusions:
Bundling of performance measurement and reporting with the admission and discharge process facilitates hospitalist performance reporting through the PQRI. The 11 PQRI performance measures relevant for hospitalists were able to be categorized for implementation, documentation, and reporting that harmonizes with the hospital admission and discharge process. The work flow around hospital patient throughput allows for a unique performance reporting strategy for hospitalists participating in the PQRI.
Author Disclosure:
P. Torcson, none; R. Slataper, none.