Case Presentation:
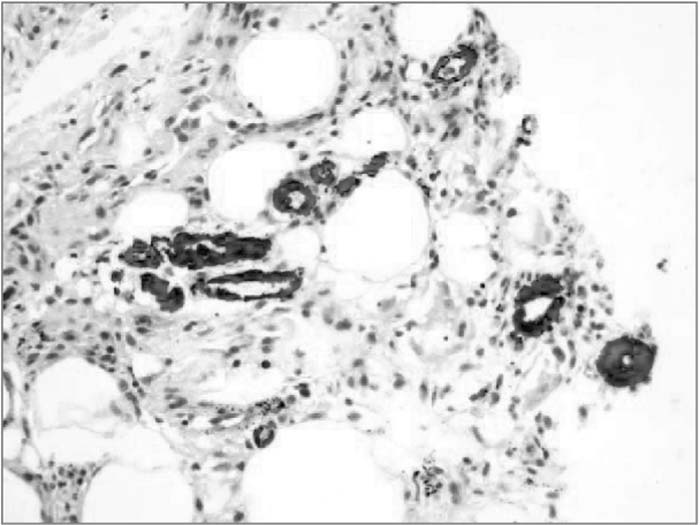
A 76‐year‐old white woman with type 2 diabetes (DM), hypothyroidism, coronary artery disease, and atrial fibrillation on oral anticoagulation was transferred to our institution with a 3‐month history of painful ulcerative lesions of her left lower extremity. The lesions had started as a rash with pruritis and progressed to nodular and ulcerating lesions with significant pain. Her medications included warfarin, calcitriol, calcium carbonate, gemfibrozil, levothyroxine, and insulin. She had been treated with courses of antibiotics and wound‐care regimens without improvement. Physical examination revealed subcutaneous nodular lesions and extensive ulcerations on the LLE. Skin biopsy revealed extensive fat necrosis and calcium deposits in subcutaneous vessels compatible with calciphylaxis. Laboratory tests revealed a corrected calcium of 8.35 mg/dL (8.5‐10.0 mg/dL), phosphate of 3.9 mg/dL (2.5‐4.5 mg/dL), PTH of 5 mg/dL (10–60 mg/dL), creatinine of 1.1 mg/dL (0.7–1.4 mg/dL), PTH‐rp < 0.2, 25(OH)vitamin D of 57.3 pg/mL (31‐80 pg/mL), and 1,25(OH)vitamin D of 18 pg/mL (22–67 pg/mL); complement levels and rheumatologic workup were normal, but homocysteine, 22 (μmol/L (3.4–12.9 μmol/L); CRP, 10,4 mg/dL (0‐2 mg/dL); and uric acid, 11 mg/dL (2‐7 mg/dL), were increased. A CT of the abdomen revealed nonobstructing renal calculi, and a CT of the brain demonstrated a small left parietal cortical infarct in addition to multiple parenchymal calcifications. The patient was started on phosphate binders to reduce phosphate levels, vitamin B and folic acid supplements to lower homocysteine, and allopurinol for the elevated uric acid.
Discussion:
Calciphylaxis (CP) has been known as a medical entity related to renal replacement therapy and hypercalcemic states. CP results in systemic medial calcification of the arteries that leads to skin and soft tissue necrosis. Recent reports demonstrate that poor kidney function and calcium abnormalities are not a requirement. Other reported etiologies include malignancy, alcoholic disease, and warfarin therapy. We present a case of rare disease in a unique context. This is the first case report of a patient with hypoparathyroidism and CP. Hypocalcemia, low calcium‐phosphorus product, and absence of rheumatologic disease and malignancy raise the question of the etiology of CP. Warfarin use could be a potential etiology; however, the prolonged use makes coumadin‐induced skin necrosis unlikely. Despite normal kidney function, elevated homocysteine and uric acid levels have been linked to arterial calcifications.
Conclusions:
Calciphylaxis is an aggressive disorder involving necrotic ulcerations that are characteristically difficult to treat. CP may be related to novel factors such as hyperuricemia and homocysteinemia. Further studies are required to evaluate if therapy directed against these metabolites will be beneficial.
Author Disclosure:
L. Oliveira, none; D. Gugliotti, none.