Case Presentation: Boerhaave’s syndrome, or effort rupture of the esophagus, is a rare and potentially life-threatening surgical emergency occurring in about 3.1/1,000,000 people per year1. We present a case of Boerhaave’s syndrome associated with cannabinoid hyperemesis syndrome (CHS).
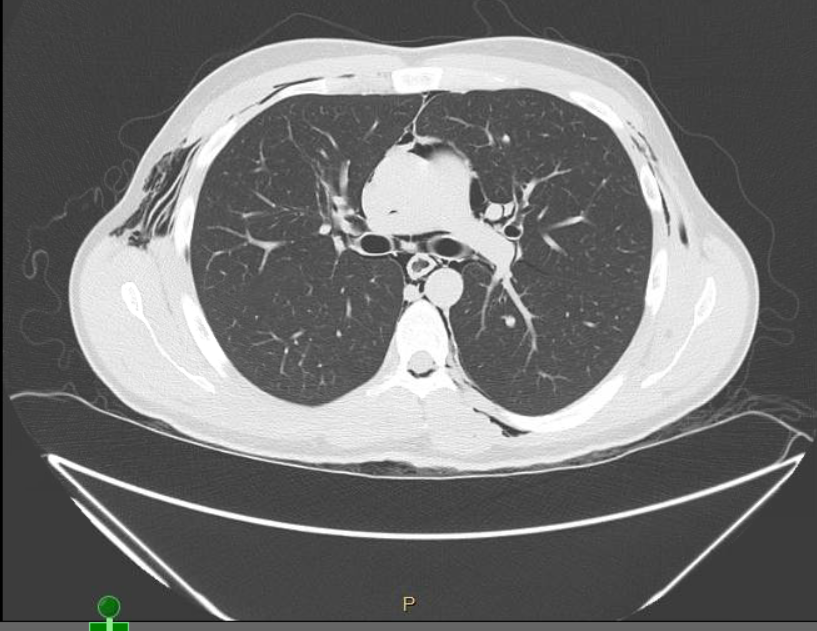
Discussion: A 21-year-old male with a history of daily marijuana use for the last 5 years presented with severe, crunching, and retrosternal chest pain after a bout of nausea and vomiting for 3 days. The patient was afebrile, hemodynamically stable, and not in acute distress. Physical exam was significant for crepitus that was palpated in the neck and upper chest area. His abdominal exam was benign. Initial blood work revealed leukocytosis of 28,000 white blood count (WBC), acute kidney injury (AKI), and lactic acidosis. A computed tomography (CT) of the chest and abdomen showed pneumomediastinum, and pneumopericardium with subcutaneous emphysema in the chest wall, lower neck, and upper abdomen. The patient was started on intravenous (IV) fluids, IV antiemetics, IV proton pump inhibitors, and broad spectrum antibiotics. Urgent gastrografin esophagram revealed 1.3 cm focus of extraluminal contrast along the left lateral wall of the lower esophagus at the gastroesophageal junction, which was suggestive of a tear. A multidisciplinary team involving gastroenterology and cardiothoracic surgery offered the patient conservative management, placement of esophageal stent versus surgical intervention. The decision was made to treat the patient conservatively with close follow up and serial imaging. A 12-hour follow-up barium study revealed no evidence of extravasation of contrast outside the esophageal lumen. The patient continued to improve symptomatically, and was discharged a few days later.
Conclusions: To our knowledge, this is the first reported case describing the association of Boerhaave’s syndrome with CHS. Most commonly, Boerhaave’s syndrome is seen with ingestion of excessive alcohol2; however, other etiologies should not be neglected, such as our case. Clinicians must be aware of the possibility of Boerhaave’s syndrome in patients with CHS, particularly when presenting with sudden, severe chest pain. Although Boerhaave’s syndrome is a full thickness perforation of the esophageal wall, it may present as a contained perforation; as in our case. Timing of diagnosis and clinical presentation are crucial in determining the management of this condition. Conservative management is usually reserved for patients with minimal symptoms, no signs of sepsis, and with the ability of contrast to flow back into the esophagus from cavity on imaging studies3. Otherwise, surgical intervention should be considered. Recently, nonsurgical options, including endoluminal stenting of esophagus, have emerged in clinical practice for cases requiring intervention based on observational studies4. However, randomized clinical trials are needed to compare the clinical outcomes between endoscopic and open surgical approaches.