Case Presentation:
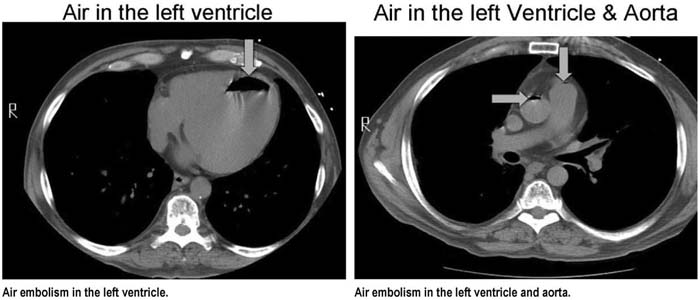
A 59‐year‐old man with a medical history significant for congestive heart failure and diabetes mellitus presented with a new right upper lobe nodule (positive on PET scan), for which he underwent a CT‐guided percutaneous biopsy. Coaxial technique was used to perform the biopsy of the more peripherally located lesion using a 19‐gauge biopsy needle. A total of 2 core biopsies were performed. During the needle pass of the second biopsy, the patient coughed and then developed hemoptysis prompting the procedure to be terminated. He was otherwise asymptomatic, with no further hemoptysis, before becoming acutely unresponsive several minutes later. He was rapidly assessed as being apneic and without a detectable blood pressure, and resuscitation efforts were begun immediately. The resuscitation was notable for repeated bouts of pulseless electrical activity and a single episode of ventricular fibrillation that responded to defibrillation. Evaluation of the patient's postprocedure CT scan, which was performed because of the hemoptysis, revealed the presence of air in the left ventricle and the aorta. Imaging also demonstrated a moderate amount of pulmonary hemorrhage at biopsy site and a small (less than 5%) right‐sided pneumothorax. The patient was intubated, placed on high FiO2 supplemental oxygen, and also placed in the left‐lateral Trendelenburg position. He did not develop any signs of systemic air embolism, and a head CT performed once he was stabilized did not reveal any signs of central nervous system embolism. He developed pneumonia, which was believed to be related to aspiration during his resuscitation. Associated acute lung injury delayed extubation for 1 week, but he was ultimately discharged home. His biopsy specimen was positive for adenocarcinoma.
Discussion:
Percutaneous transthoracic needle biopsy is a common procedure for evaluating lung lesions. The most frequent complications include pneumothorax, hemorrhage, and hemoptysis. The formation of a communication between an airway and a pulmonary vein is the presumed mechanism of air embolization resulting from percutaneous lung biopsy. It is possible that the fluctuations in intrathoracic pressure and/or direct needle trauma created by the coughing episode in our patient contributed to the entry of air into his pulmonary veins. Positioning of patients after this complication remains controversial. Rapid application of 100% oxygen for the affected patient can promote resorption of the embolized air, as was seen in our patient. Hyperbaric oxygen therapy is also currently regarded as a mainstay of therapy for affected patients as it increases the rate of resorption of the embolized air.
Conclusions:
Clinicians should be aware of this unusual complication following percutaneous lung biopsy, as early recognition leads to improved outcomes.
Author Disclosure:
S. George, none; M. Bolu, none: A. Marte‐Grau, none; R. Bobba, none; T Martin, none.