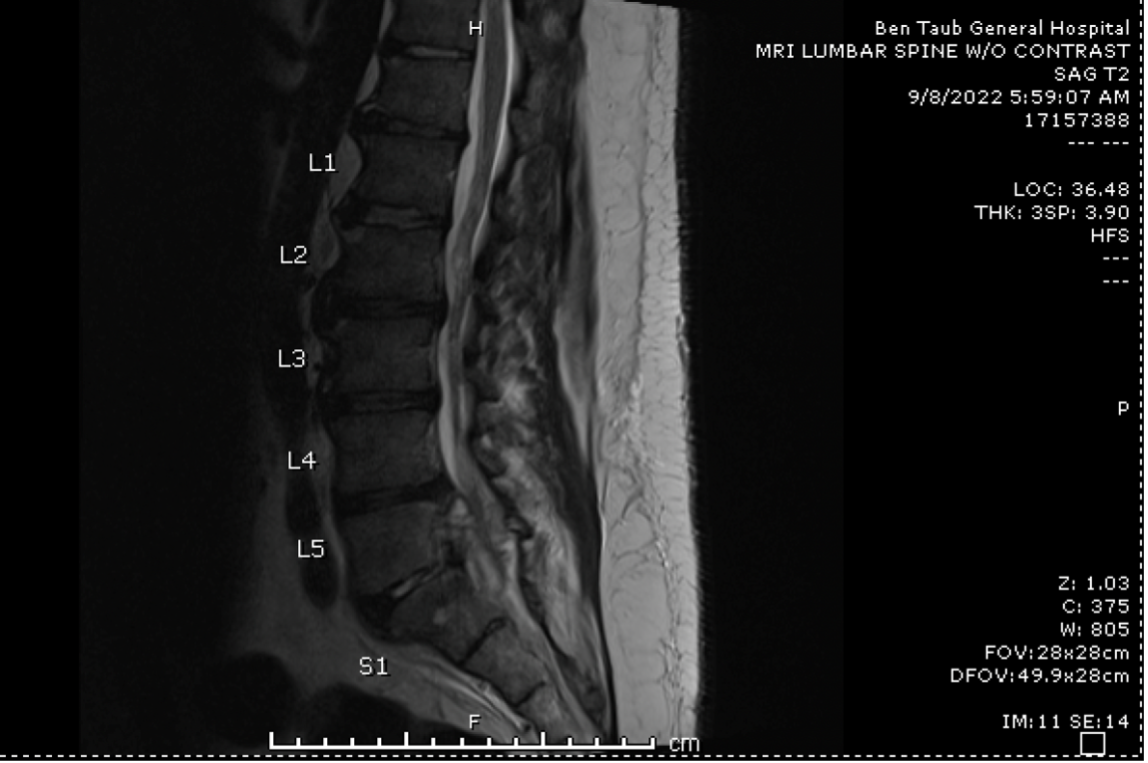
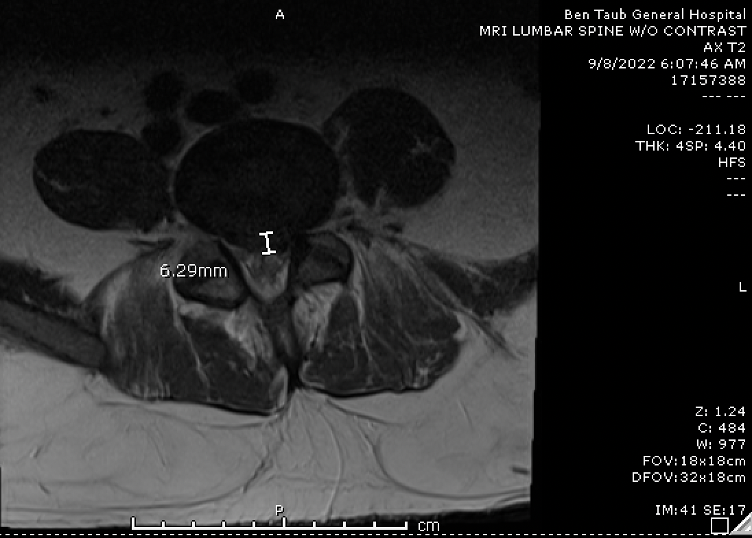
Case Presentation: The patient is a 36 year-old man with no significant past medical history who presented with 1.5 months of worsening left sided low back pain and sciatica that rapidly progressed to bilateral leg weakness. Three days prior to presentation, he lost his ability to ambulate and had an episode of fecal incontinence associated with saddle anesthesia. The patient immigrated from Mexico 7 months ago and had no known exposure to farm animals. Although he initially denied consuming unpasteurized dairy products, he later revealed that his relatives recently brought him cheese from Mexico. His initial laboratory workup revealed an elevated ESR of 67 mm/hr, and an unremarkable CRP, BMP, and CBC. MRI without contrast demonstrated spondylodiscitis in L5-S1 as well as evidence of phlegmon extending from L4-S3 (Figure 1). He underwent a laminectomy, incision and drainage, and spinal revision. Blood cultures revealed Brucellosis abortus. Serum Brucella IgM and IgG were also positive. Abscess cultures showed no growth. He was initiated on a 2-week course of IV Gentamicin 400 mg once daily along with Doxycycline 100 mg and Rifampin 900 mg daily for 3-6 months.
Discussion: Brucellosis is a systemic zoonotic infection that is endemic to South and Central America, the Middle East, and eastern Mediterranean countries [1,4]. Individuals at risk for infection include those who have direct contact with infected animals, consume raw or unpasteurized dairy products from an infected animal, or inhale infected aerosolized products [6]. Blood cultures, the diagnostic gold standard, are positive in 25% – 80% of cases and can take up to 10 days or longer to isolate. One of the most common complications of Brucellosis is spondylodiscitis which often involves the lumbar spine and has an incidence rate of 10% [4]. A rarer complication is the development of a spinal epidural abscess which can lead to permanent neurologic deficits, including paraplegia or quadriplegia. Brucellosis spondylodiscitis is a difficult condition to treat. In a review of 303 patients with Brucellosis spondylodiscitis across 8 different studies, 22.77% failed treatment with a prolonged antibiotic regimen [3]. Currently, there is no consensus on the antibiotic regimen to use for these patients. Common regimens include combination therapy with Doxycycline plus Streptomycin, Rifampin, newer aminoglycosides, TMP-SMX, or fluoroquinolones. In terms of duration of treatment, patients who receive greater than 12 weeks of therapy experienced a significantly higher rate of treatment success compared to those who received 6 weeks of therapy or less [3]. There is, however, no consensus on whether these patients should receive medical management alone versus medical plus surgical management, though those who present with cord compression, such as our patient, should undergo emergent surgical intervention due to risk of permanent paralysis.
Conclusions: This case presents Brucellar spondylodiscitis with spinal epidural abscess in a young and immunocompetent patient. Although rare, it is important for clinicians to recognize Brucellosis as a potential cause of spinal epidural abscesses in patients with functional immune systems. Clinicians should also be aware that a negative culture does not necessarily preclude Brucella as the causative pathogen and that further serologic testing may be needed to assist with diagnosis. Furthermore, prompt treatment is of the utmost importance to prevent permanent neurologic sequelae.