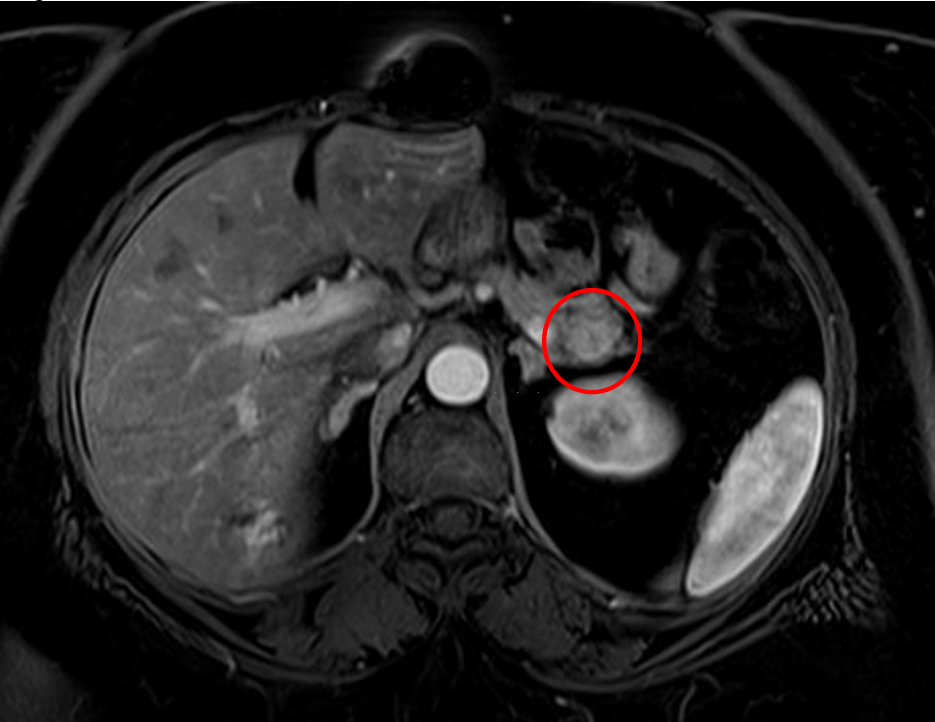
Case Presentation: A 65 year old woman with hypertension, hyperlipidemia, and gastric bypass surgery in 2005 presented to the emergency department with episodes of confusion. Four years prior to her presentation she began to have episodes of confusion where she would stare off into space and it was noted that eating relieved these symptoms. She saw a neurologist and had a normal EEG and CT head. On the day of presentation, she ate lunch at noon and then went to her dentist appointment in the late afternoon. At the appointment she had an episode of confusion with facial numbness/tingling. She was provided some juice with relief, and decision was made to bring her to the emergency department. She had stable vital signs on arrival. Initial labs were notable for glucose of 36 mg/dL which improved to 114 mg/dL after an ampule of D50. CT head was unremarkable. A few hours later she had recurrent hypoglycemia of 49 mg/dL and was provided food with improvement. A monitored fast was initiated upon admission and with the next episode of hypoglycemia her insulin, pro-insulin, and c-peptide were measured, all of which were within normal ranges. She had a negative sulfonylurea screen and normal TSH and cortisol. An MRI of her abdomen was obtained which noted a 15 mm solid hypervascular mass in the tail of her pancreas concerning for neuroendocrine tumor. She underwent EGD and EUS with fine needle biopsy with pathology noting features suspicious for neoplasm. She then underwent a splenectomy, distal pancreatectomy, and cholecystectomy with pathology noting a well differentiated neuroendocrine tumor in the distal pancreas. It was also noted that she had several areas of nesidioblastosis, and despite negative margins there was concern for future recurrence of hypoglycemia. She was discharged and has not had readmissions for recurrent hypoglycemia in the subsequent 7 months.
Discussion: Insulinomas are rare with an incidence of ~4/1,000,000. They can occur anywhere in the pancreas and are often solitary lesions. As in this patient, a normal insulin level does not preclude the diagnosis as total absolute level may not be elevated. Initial work up includes CT, MRI, EUS, or intra-arterial calcium stimulation test and hepatic venous sampling. Both solitary and metastatic lesions are treated with surgical resection when possible. Treatment of metastatic disease is aimed at preventing hypoglycemia with octreotide and continuous glucose monitoring.Nesidioblastosis is the proliferation of pancreatic ductules which can lead to hyperinsulinemia. It is rare in adults and it is a separate entity from insulinoma. Treatment is controversial, and can include a low carbohydrate diet, octreotide, and in some patients pasireotide. Surgical resection is considered for many patients as well.
Conclusions: Recurrent hypoglycemia should evoke a broad differential for a hospitalist, including rare causes such as insulinomas. If imaging is without a notable mass, nesidioblastosis should be considered as a cause of recurrent hypoglycemia.