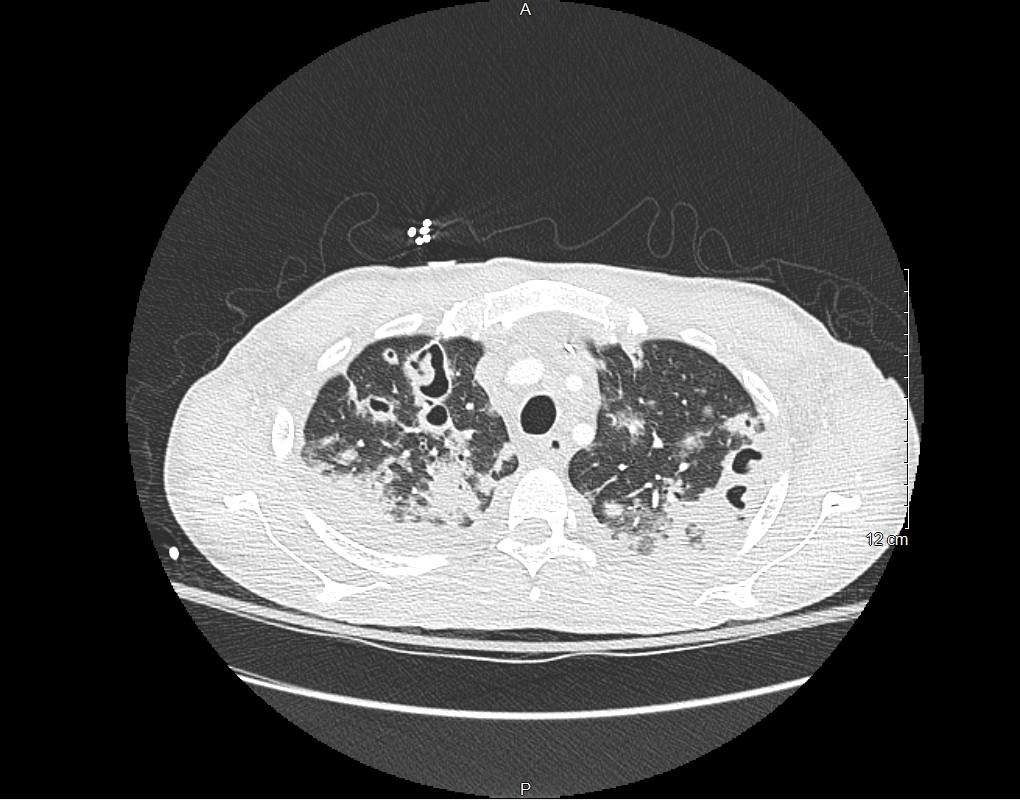
Case Presentation: 29-year-old Hispanic male with history of intravenous drug use (IVDU) with fentanyl and methamphetamine, was brought to the hospital after being found confused on the streets. Patient was very cachectic, tachypneic and had track marks in the cubital fossa suggestive of IVDU. Patient was febrile with 100.6 F, had leukocytosis with WBC 18 K and Creatinine 2.3mg/dL. He was hypoxic, hypotensive and encephalopathic. CXR showed bilateral peripheral airspace opacities suggestive of multifocal pneumonia. Computed tomography of chest showed extensive multifocal areas of consolidation and cavitary nodular opacities within both lungs. Findings were indicative of severe multifocal pneumonia with necrotizing changes. Abdominal ultrasound showed hepatosplenomegaly. HIV antibody was reactive. Hepatitis C antibody was reactive. Patient was started on broad spectrum antibiotics including Vancomycin and Meropenem. Atovaquone was added for PCP prophylaxis. Methicillin-susceptible Staphylococcus Aureus MSSA was isolated in 2 sets of blood cultures. Patient was switched to IV Oxacillin. Transthoracic echocardiogram showed tricuspid valve vegetation measuring 1.6 x 1.5 cm and normal systolic function. Patient was diagnosed with right-sided tricuspid valve endocarditis with septic pulmonary embolism. Tuberculosis spot test was negative. Sputum Acid fast bacilli (AFB smear) and culture was negative. Cryptococcal antigen was negative. HIV PCR showed > 242 K Cp/ml with CD4 count of 556 /cu mm. Patient had a long hospital course with worsening hypoxia, requiring mechanical ventilation. He was initiated on hemodialysis for renal failure and required multiple vasopressors for shock. Patient continued to decline and passed away.
Discussion: Right-sided infective endocarditis (IE) accounts for approximately 10% of all cases of IE, and is predominantly encountered in intravenous drug users. Epidemiological data reveal a steep rise in the hospitalizations for intravenous drug use IVDU-associated IE over the last few decades. With the rise in incidence of IVDU-associated IE, mortality due to IE among young adults with substance use disorder has increased significantly. The diagnosis of right-sided infective endocarditis is challenging, resulting in delay in initiation of appropriate treatment, which in turn adversely affects the outcome. Right-sided IE differs from left-sided IE in terms of clinical presentation, diagnostic findings and prognosis; hence they require different management strategies. Cardiac murmurs and systemic emboli are usually absent in right-sided IE, whereas pulmonary embolism and its related complications are the predominant clinical features. Septic pulmonary emboli with or without cavitations, occur in more than half of the patients with right-sided IE. Cavitary lung lesions in intravenous drug user should raise concern for right-sided IE and septic emboli. Infective endocarditis with pulmonary complications is associated with worse outcomes including mortality and necessitates timely management.
Conclusions: Right-sided infective endocarditis poses a significant challenge to medical practitioners. Compared with extensive data on left-sided infective endocarditis, there is much less published information on the features and management of right-sided IE and hence require future efforts. Right-sided IE should be highly considered when encountering a patient with IVDU who presents with fever, bacteremia, respiratory symptoms and pulmonary infiltrates.