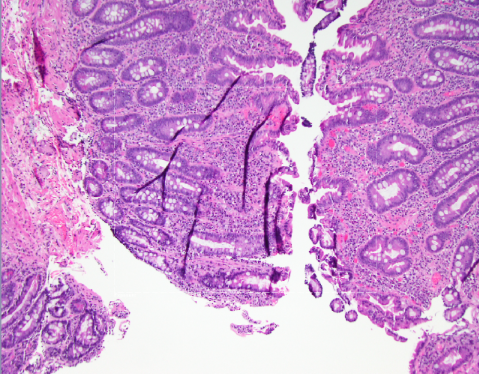
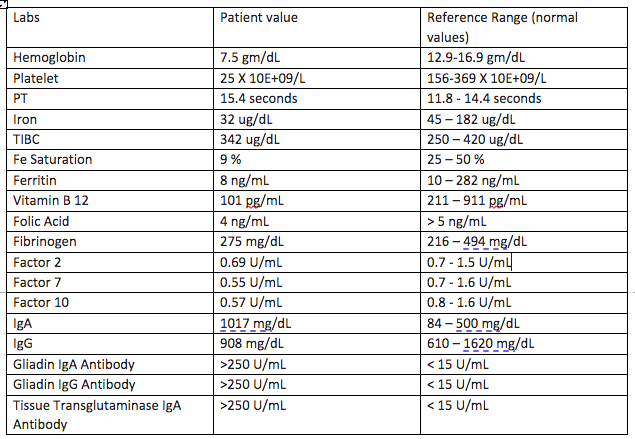
Case Presentation: 62-year-old male with a PMH notable for recurrent epistaxis, bleeding post-dental procedures & IDA since childhood on & off oral iron supplementation presented to the hospital with a traumatic head injury resulting in a SAH/SDH. Initial laboratory work found normocytic anemia & severe thrombocytopenia (TCP) – 25 X 10E+09/L . CT abdomen & pelvis ruled out splenomegaly or any liver abnormality. Peripheral blood smear showed morphologically normal platelets & no schistocytes. Flow cytometry was non-specific and a bone marrow biopsy was completed which showed mildly hypocellular marrow with trilineage hematopoiesis, no increase in blasts and a mild increase in plasma cell. Iron staining done on bone narrow sample showed adequate storage iron with no ring sideroblasts. Extensive workup was grossly unremarkable & TCP was attributed to ITP as a diagnosis of exclusion. Though the patient did not have any signs & symptoms of malabsorption, he was found to be deficient in multiple vitamin & minerals on routine lab work. This prompted further work-up for malabsorptive processes such as celiac disease (CD) despite the patient have no symptoms pointing towards malabsorption. Finally, an esophagogastroduodenoscopy (EGD) with biopsy & celiac panel both confirmed the diagnosis of CD.Patient was recommended to start a gluten-free diet & was initiated on Intravenous iron infusion, folic acid, & vitamin B12 supplementation. Over the course of hospitalization, the patient received platelets with poor response as typically seen with ITP. Eventually, the patient received Intravenous Immune Globulin (IVIG) inpatient & was initiated on oral steroids. Repeat blood work continued to show worsening thrombocytopenia & patient was started on eltrombopag with good response.
Discussion: Poly-autoimmunity is the presence of more than one autoimmune condition in a patient [2]. Numerous studies have investigated the frequency of association between similar autoimmune disorders. Although there have been many case reports discussing the co-occurrence of CD & autoimmune thyroid disease [3], limited data is available on CD & ITP. A prospective observational study performed on 261 patients with celiac disease & 32 patients with ITP, the result of which indicated that there truly is “a greater frequency of ITP in celiac disease & vice versa” [1]. The prevalence of celiac disease is on the rise. This enteropathy occurs in the setting of an autoimmune response to gluten. Symptoms include diarrhea, abdominal pain, bloating, weight loss and failure to thrive. Diagnosis is based on serological testing & intestinal biopsy. Management consists of a gluten free diet. ITP, presence of a low platelet count due to antibody-mediated platelet destruction, is commonly a diagnosis of exclusion. Our patient with ITP with no gastrointestinal symptoms was found to have multiple nutritional deficiencies attributed to CD. Our case highlights the unique correlation between ITP and CD which is rarely seen.
Conclusions: Poly-autoimmunity, a phenomenon of co-occurrence of multiple autoimmune diseases, should be considered in patients with a solitary autoimmune disorder. Physicians should keep in mind that sometimes a benign disorder like ITP can be intensified and difficult to treat in the presence of other autoimmune disorders such as CD. The question remains still; should all patients with ITP be screened for other autoimmune disorders? Lack of established guidelines makes it difficult to draw conclusions and more research is needed in the field.