Background: Previous work suggests that hospitals’ teaching status is correlated with readmission rates, cost of care, and mortality. This research has focused on conditions closely tracked by the Centers for Medicare and Medicaid Services (CMS). The extent to which hospitals’ teaching status impacts care processes for syncope has not been extensively studied.
Methods: We merged data from the Healthcare Utilization Project (HCUP) State Inpatient Databases (SID) and the American Hospital Association (AHA) Annual Survey, looking at inpatient management for admissions with a primary diagnosis of syncope in Maryland and Kentucky for years 2008-2014.
We created regression models to identify hospital characteristics associated with cardiac ischemia evaluations (i.e. stress test or cardiac catheterization).
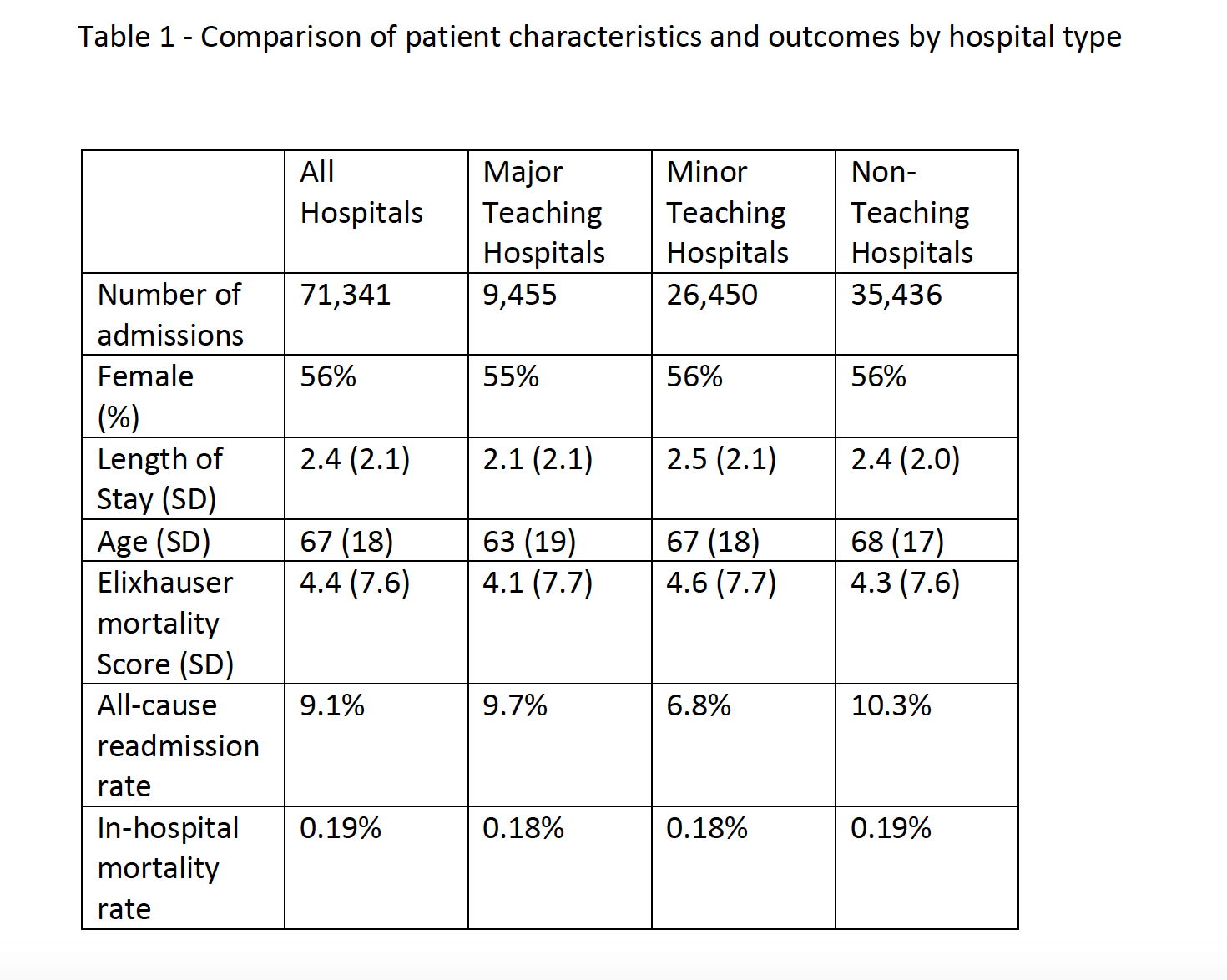
Results: The merged dataset included 71,341 syncope admissions at 151 hospitals.
Non-teaching and minor teaching hospitals had a slightly longer LOS relative to major teaching hospitals. All-cause readmission rates were lower for minor teaching hospitals than for non-teaching and major teaching hospitals (table 1).
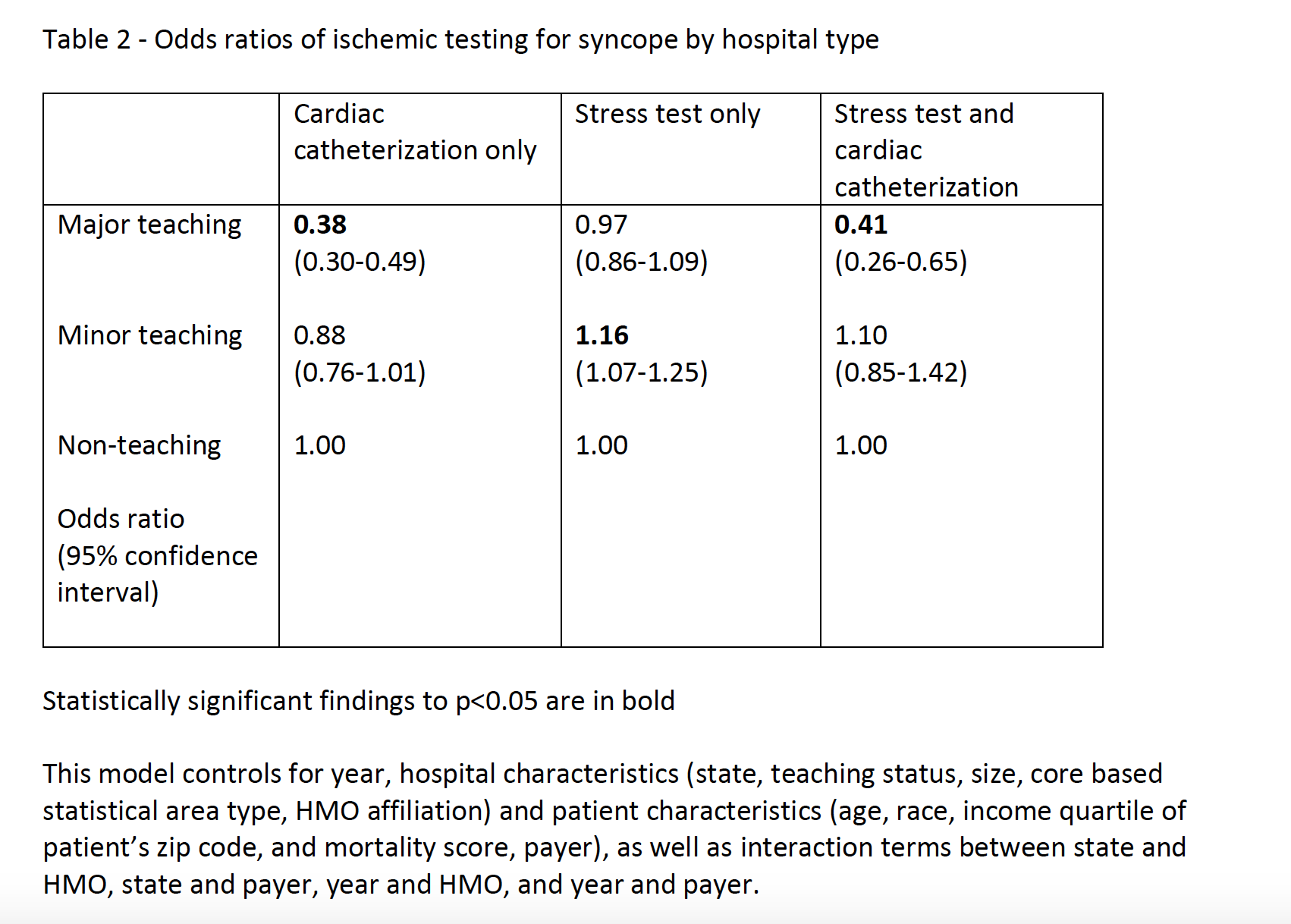
Controlling for patient sociodemographic factors and hospital characteristics, there was a significantly lower likelihood of cardiac catheterization at major teaching hospitals relative to non-teaching hospitals (table 2).
Overall, 15% of patients had an ischemic evaluation. However, fewer than 0.3% of patients had a secondary or tertiary diagnosis of acute MI.
Conclusions: It is likely that a significant percentage of the cardiac catheterizations performed on patients with a principal diagnosis of syncope represents overuse, as fewer than 0.3% of these patients also had a troponin elevation. Moreover, only 9% of stress tests were followed by cardiac catheterization, suggesting that the number that were positive was relatively low. We do not know what percentage of these cardiac catheterizations actually led to an intervention.
Our study shows that patients admitted for syncope to a major teaching hospital are significantly less likely to undergo cardiac catheterization, a procedure that is likely low-value. Further efforts to understand what incentives underlie this trend and to replicate them at minor teaching and non-teaching hospitals should be undertaken.