Background: Sepsis research is limited by heterogeneity and inaccuracy of patient identification. An ideal identification algorithm would broadly define a population with suspected infection to optimize discrimination and provide real-time identification of high-risk populations for potential interventions. We combined clinical and administrative to identify a population of adults hospitalized with suspected infection and examined characteristics and outcomes.
Methods: We retrospectively selected adults who were admitted as inpatient or observation (IP/OBS) from January 2014 to May 2017 at 16 Carolinas HealthCare System (CHS) facilities with any of the following 3 criteria: (i) any diagnosis code associated with infection (Diagnosis); (ii) anti-infective order (Rx); or (iii) a microbiology order (Micro), e.g. culture or polymerase chain reactions. Populations were compared by the different combinations of methods used to identify suspected infection. The population was characterized by demography, Charleston Comorbidity Index (CCI), and qSOFA score within 24 hours after admission. Outcome measures included 30, 60, and 90-day mortality and readmission rates (IP/OBS).
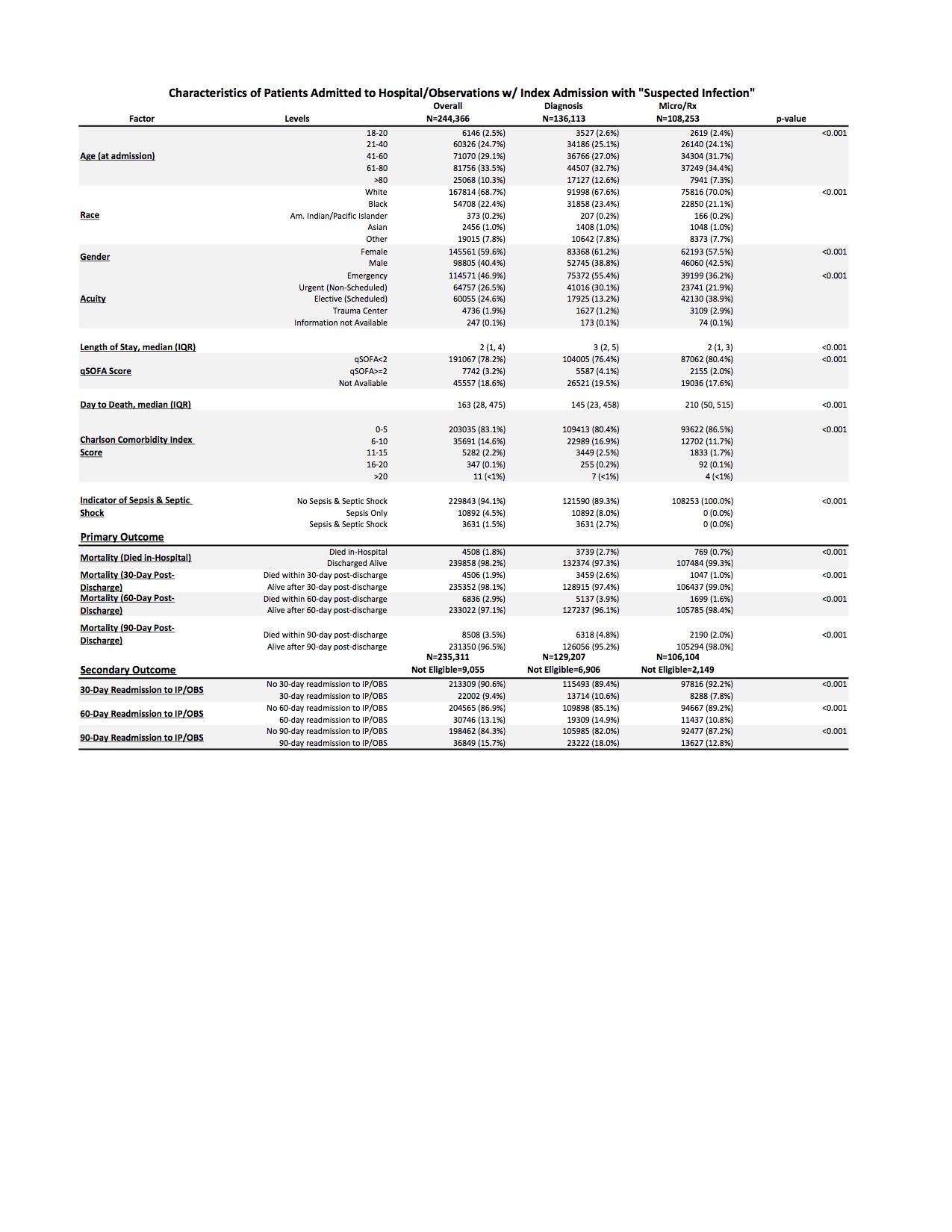
Results: 244,366 patients met any of the 3 inclusion criteria (Overall), 136,113 (55.7%) were identified by diagnosis and 108,253 (44.3%) by Micro/Rx. In the Overall group, 4.5% had a diagnosis code for sepsis and 1.5% for septic shock compared to 8% and 2.7% respectively in the Diagnosis group and 0% and 0% in the Micro/Rx group. CCI scores between 0 and 5 were 83.1% (Overall), 80.4% (Diagnosis), and 86.5% (Micro/Rx). Patients with qSOFA scores >=2 were 3.2% (Overall), 4.1% (Diagnosis), and 2% (Micro/Rx). Mortality rates of in-hospital, 30, 60, and 90 days post discharge were 1.8%, 1.9%, 2.9%, and 3.5% respectively in Overall group, 2.7%, 2.6%, 3.9%, and 4.8% in Diagnosis, and 0.7%, 1%, 1.6%, and 2% in Micro/Rx. Among the overall study cohort, 235,311 patients were eligible for readmission analyses. Of these, 9.4%, 13.1%, and 15.7% were readmitted to IP/OBS within 30, 60, and 90-day, respectively. The Diagnosis group again had higher rates comparatively on 30, 60, and 90-day readmission to IP/OBS (10.6%, 14.9%, and 18% respectively). See Table 1 for additional characteristics.
Conclusions: Compared to using diagnosis code alone, including triggers for microbiology and anti-infectives defines a broader and more complete population of patients with suspected infection. This identification algorithm is more expansive than diagnosis codes alone, and thus identifies a population at lower risk for morbidity (readmission) and mortality. Importantly, a comprehensive approach like this provides the foundation for a more powerful opportunity to explore factors placing patients at risk for morbidity and mortality related to sepsis.