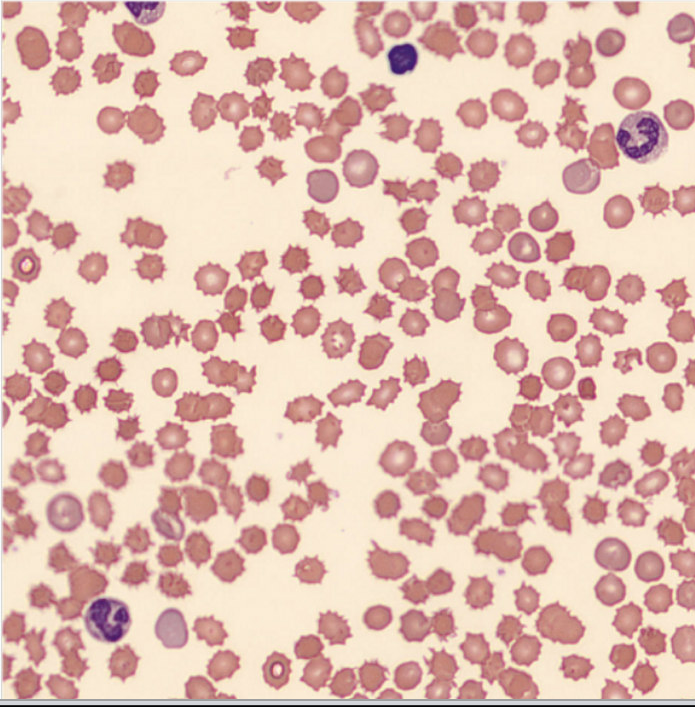
Case Presentation: A 23-year-old man with alcohol use disorder presents with abdominal swelling, lower extremity edema, jaundice, and early satiety. Physical examination revealed icteric sclera, conjunctival pallor, distended abdomen with notable ascites, and lower extremity edema. Initial labs showed macrocytic anemia at 7.5 g/dl with mean cell volume of 127.2 fL, white blood cell count of 10.4 cells/mm³, and platelet count of 74,000 cells/mm³. Further analysis of the anemia showed signs of hemolysis: elevated absolute reticulocyte count 319,000/µL, haptoglobin < 10, indirect hyperbilirubinemia, and increased lactate dehydrogenase. The direct Coombs test, thyroid-stimulating hormone, vitamin B12, and folate levels were normal. A peripheral blood smear revealed numerous acanthocytes, suggesting spur cell anemia (see figure), and an abdominal ultrasound showed liver cirrhosis, splenomegaly, and ascites. A lack of health insurance precluded the patient from receiving a liver transplant. He was trialed on steroids as reports have shown them to be effective in spur cell anemia, but was discontinued due to sepsis. He was ultimately managed conservatively with diuretics and large-volume paracentesis and now follows up at the hepatology clinic.
Discussion: Anemia is common in patients with liver cirrhosis, with a reported prevalence of 50-87%(1). The etiology of anemia in liver cirrhosis is multifactorial: direct blood loss from gastrointestinal bleeding due to esophageal varices, peptic ulcer disease, and portal hypertensive gastropathy; coagulopathies; malnutrition leading to nutritional deficiencies; and anemia of chronic disease, since the liver secretes hepcidin in these states(2). Hemolytic anemia in liver cirrhosis occurs in hypersplenism from portal hypertension, autoimmune hemolytic anemia from autoimmune hepatitis, and rare causes such as Wilson’s disease and Zieve syndrome. Spur cell anemia (SCA) is a rare cause of acquired hemolytic anemia seen in advanced liver cirrhosis. It is associated with poor prognosis and a high 90-day mortality (3). SCA is defined by more than 5% of acanthocytes on a blood smear. These are red blood cells with spicules of varying lengths without central pallor. Reduced activity of lecithin: cholesterol acetyltransferase due to liver cirrhosis alters red blood cell membrane phospholipid metabolism, causing abnormal membrane projections that are removed by the spleen, leading to spur cell formation, increased membrane rigidity, and accelerated destruction by splenic macrophages(4).Definitive treatment of spur cell anemia is an orthotopic liver transplant(5). Spur cell anemia is often resistant to blood transfusions, as transfused red blood cells rapidly acquire the abnormal spur cell shape due to the persistently abnormal lipid profile(6). Steroids have been reported to be effective in SCA(7). Steroids may have reduced the burden of hemolysis; however, the increased risk of sepsis is a limiting factor, as seen in the patient. General supportive measures for managing liver cirrhosis, unfortunately, do not reduce spur-cell anemia in cirrhotic patients.
Conclusions: Anemia frequently occurs in liver disease, and its causes are often multifactorial, necessitating careful analysis to identify the etiology. Spur cell anemia is a rare type of hemolytic anemia. Our goal is to increase awareness of SCA and explore conservative management strategies when a liver transplant is not available.