Background: Direct admissions (DA), wherein patients are non-emergently admitted to the hospital, bypassing the emergency room (ER), makeup 15% of non-elective adult hospitalizations (1). DAs can reduce ER volumes (2), but may lead to delays in initial evaluation of patients and inappropriate admissions (2,3). DAs carry risks involved with transitions of care and handoffs, yet little focus is given to the outpatient to inpatient transition. Implementation of a standardized DA handoff tool may improve the transition of care for DA patients.
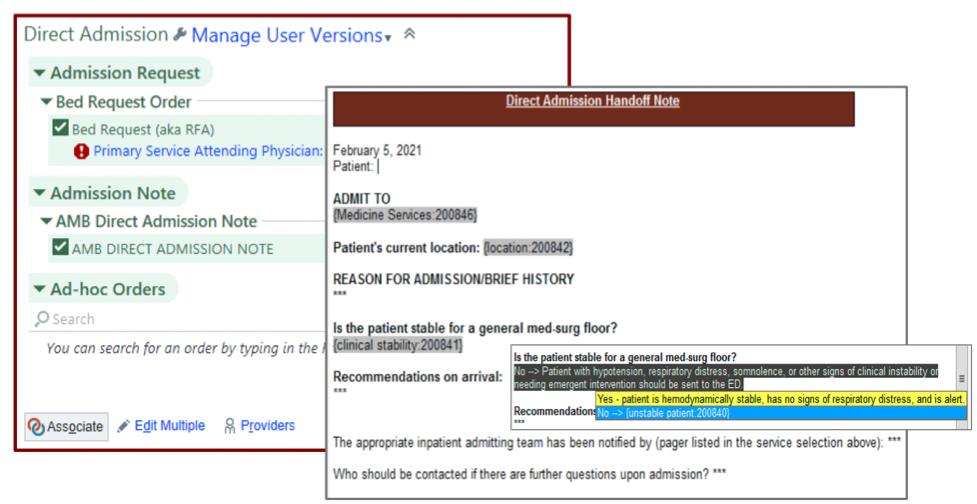
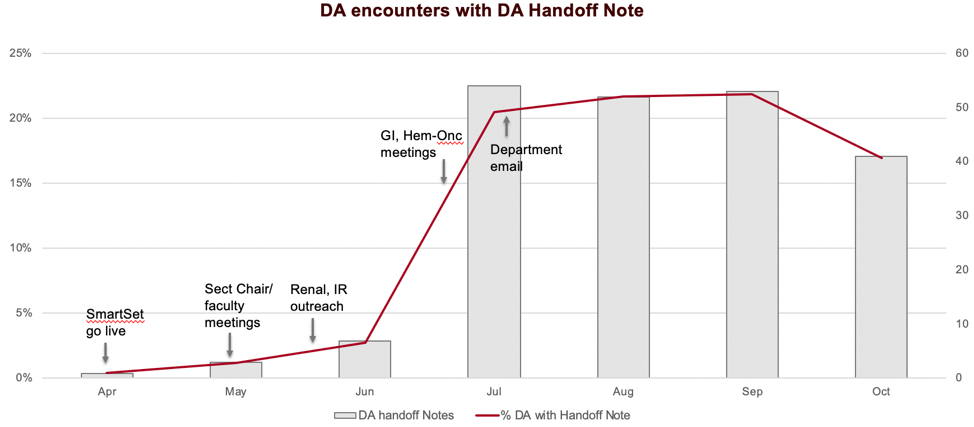
Methods: This quality improvement (QI) project was conducted at a large academic hospital over 12 months (November 2021-2022) and involved inpatient and outpatient providers in the Department of Medicine (DoM). A current state assessment of the DA handoff process was conducted via a convenience survey of internal medicine residents (IMR) and hospitalist physicians. Survey questions included multiple choice and a 5-point Likert scale querying the inpatient physicians’ perspective on promptness of DA communication, frequency of verbal and written handoffs, and satisfaction with elements of the DA process (general state, quality of handoff information, timing of handoffs, ability to reach outpatient providers, clinical stability on arrival). Write-in options were also included. Responses were reported using descriptive statistics. Next, we created an electronic medical record (EMR) note template [Fig. 1] via an Epic EMR “SmartText” to prompt outpatient providers to document key information (ascertained from inpatient providers’ feedback). We developed an Epic “SmartSet” or ambulatory order set to link the handoff note to a bed request order, a necessary step of the DA process [Fig. 1]. The DA SmartSet displayed as a suggested SmartSet for targeted DoM sections and included “bed request” synonyms for likelier retrieval on searches. For outreach, we presented current state survey data, introduced the handoff tools at DoM leadership, faculty, and targeted section meetings, and sent a leadership-endorsed DoM-wide email [Fig. 2]. DA Handoff note use and DoM monthly DA data were obtained through Clarity and Epic workbench reports respectively.
Results: Of the 188 IMR and hospitalists surveyed, 45 (24%) responded. 69% of respondents were unsatisfied with the current state of DA, 62% were unsatisfied with the ability to communicate with outpatient providers, and 69% were unsatisfied with the quality of handoff information. For write-in questions, respondents identified unstable vital signs on arrival, inadequate handoff information (i.e. no reason for admission or immediate next steps), delays in treatment, and late notification of patient arrival as safety hazards.Usage of DA handoff notes climbed from 0 at the start of implementation (April) to a peak of 55 encounters in July (20% of total DoM DA encounters). Note usage was sustained in August and September (22%) but slightly decreased in October (17%) [Fig. 2].
Conclusions: We identified deficient or absent outpatient to inpatient handoffs as a key dissatisfier and safety concern for inpatient physicians who see DAs. The use of a standardized note template and order set is feasible to implement standardized, documented handoffs for DA, and is sustainable. Future Plan-Do-Study-Act cycles will include determining individual DoM section user rates for targeted outreach, incorporating user feedback to improve ease of use and uptake of the tool, and conducting a post-intervention survey.