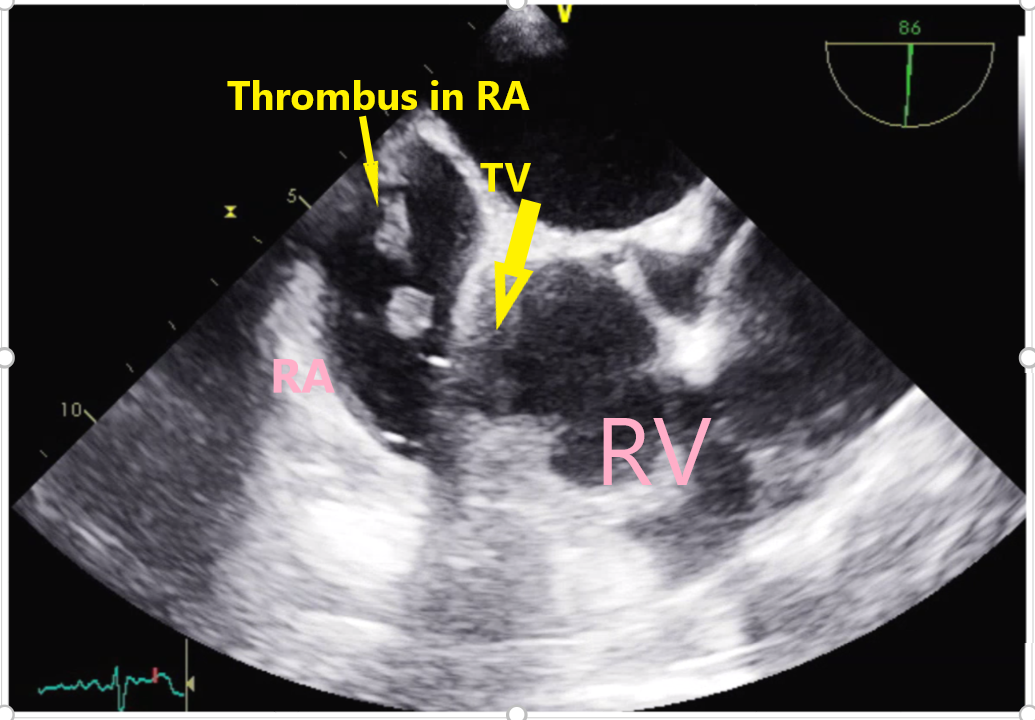
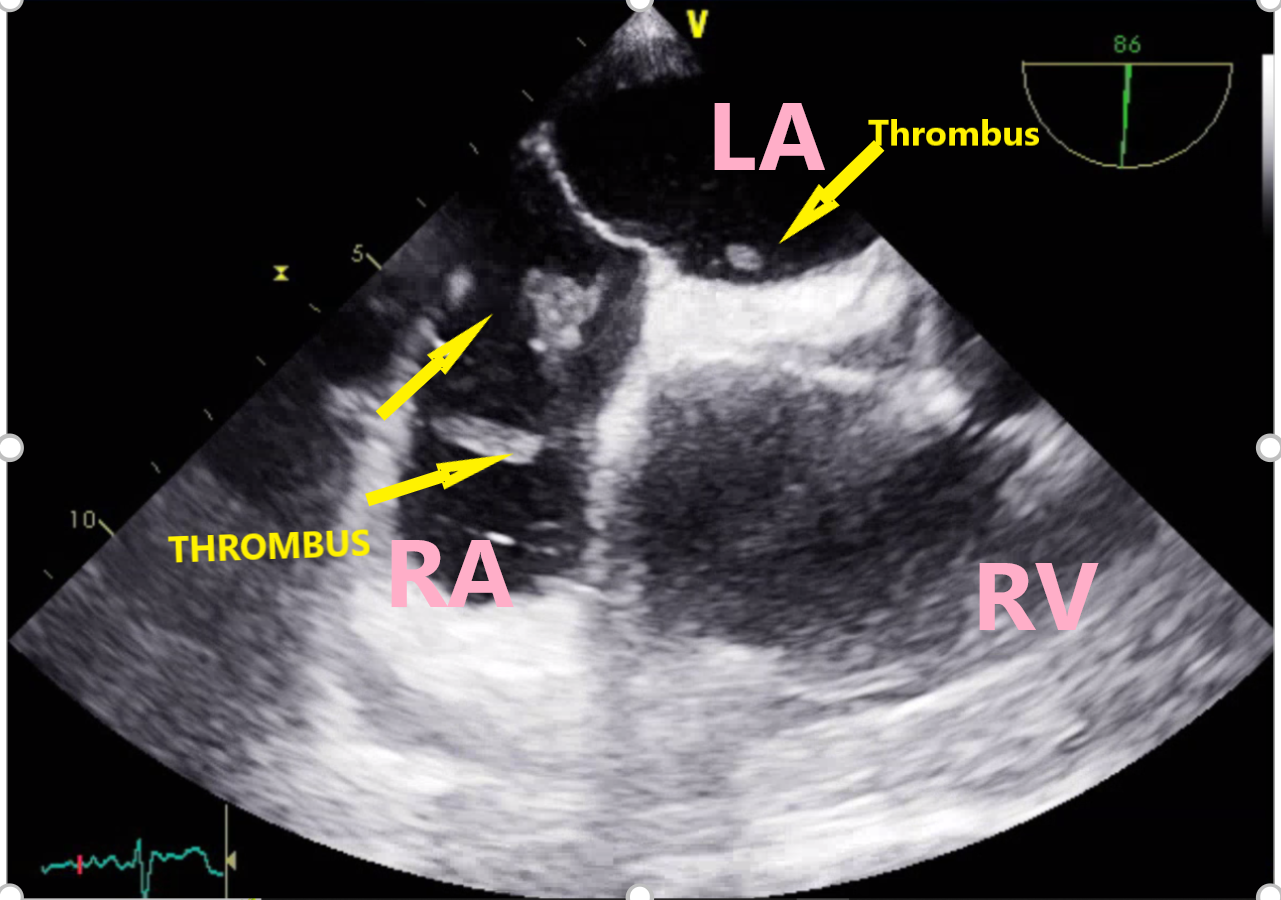
Case Presentation: 70-year-old female with past medical history of vascular dementia, recent COVID infection (three weeks before) was brought from nursing home for altered mental status, one episode of vomiting and hypoxia as per the records. On arrival she was hypotensive to 71/43 mm Hg requiring norepinephrine, heart rate 118 beat/minute, saturating 94% on 2L, and temperature 37.7°C. Physical examination significant for hypersomnolence; icterus; irregular and tachycardic pulse, pedal edema 1+; right upper quadrant tenderness. Labs notable for leukocytosis 28 X109/L, ALT 87 U/L, AST 115 U/L, ALP 253 U/L, GGT 226 U/L, Creatinine elevation of 1.5 mg/dl, glucose > 500 mg/dl with negative beta-hydroxybutyrate. Electrocardiogram identified atrial fibrillation with a rapid ventricular rate. She was intubated for escalating oxygen requirement and started on broad-spectrum antibiotics and transferred to the intensive care unit. CT (Computerized Tomography) of abdomen concerning for cholangitis. Percutaneous transhepatic cholecystostomy tube was placed and ERCP was planned next day. Transthoracic echocardiogram was done on day two, and showed increased echogenicity in the right atrium suggestive of thrombus in transit, right heart strain. CT angiography of chest revealed large acute pulmonary emboli (PE) in the segmental and subsegmental lesions of upper and lower lobes with right heart strain. Anticoagulation withheld until ERCP done which drained pus with sludge, and stone was removed followed by sphincterotomy/ampullary dilatation. After the procedure heparin drip was started for VTE. On day three, the septic shock resolved and the transaminitis started resolving and the patient was extubated. Transesophageal Ultrasound (TEE) showed highly mobile thrombus arising from the vena cava and within the right atrium with portion of it prolapsing in the tricuspid valve in diastole as seen in image 1. It also appeared to cross the Patent Foramen Ovale (PFO) to the left atrium as seen in image 2. After an interdisciplinary meeting with pulmonary critical care, interventional cardiology she was considered very high risk for clot retrieval given the presence of PFO and septic shock. The options of catheter-based therapy, systemic tPA vs conservative management with anticoagulation was given, and given the patient had dementia the family proceeded with anticoagulation and observation. The patient continued to get clinically better within five days of admission and was later discharged to her nursing home on oral rivaroxaban.
Discussion: Clot in transit is a rare venous thromboembolic (VTE) phenomenon and often in conjunction with PE has high mortality up to 40% (1). COVID-19 infection was found to be a pro-inflammatory state causing catastrophic events even in the patients who did not have significant lung injury and required intensive unit care initially (2). There are various modalities of treatment that could be employed for such catastrophic VTE, the best being catheter-based clot retrieval (3). The other options include systemic administration of thrombolytic therapy versus anticoagulation, the choice of which would depend on the acuity of the patient, type of facility, and availability of interventional cardiology and pulmonary embolism team.
Conclusions: This case highlights the importance of low suspicion of VTE in early or late stages of COVID-19 and the challenges a physician might face for the treatment of the clot-in-transit.