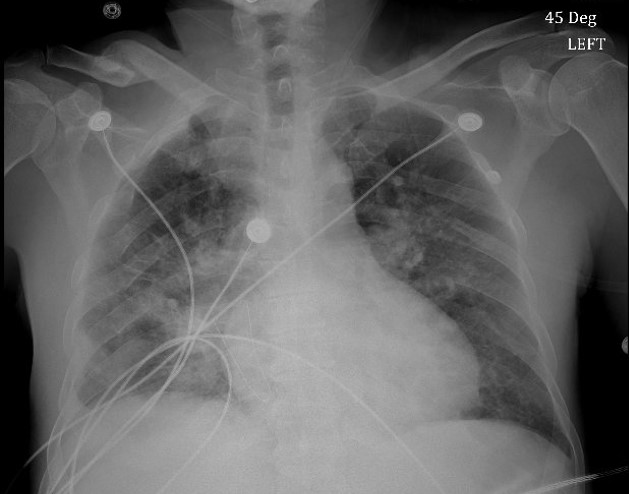
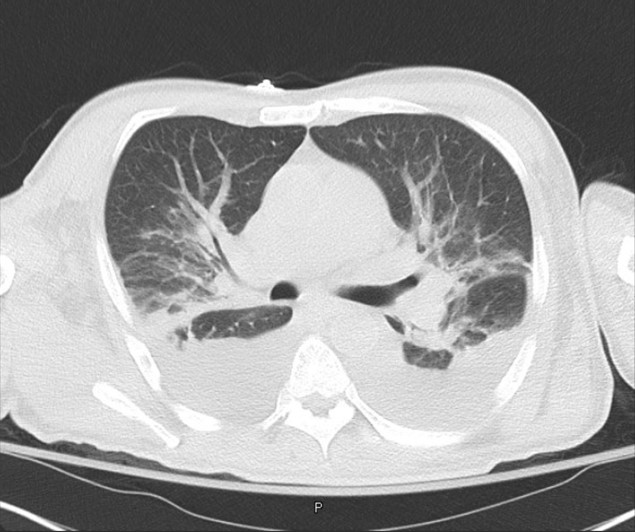
Case Presentation: A 51-year-old Hispanic male with Type 2 diabetes mellitus and dyslipidemia was admitted from the ED for evaluation of recurrent fevers, multiple joint pains, and tachycardia. Physical exam findings included cachectic appearance and right inguinal lymphadenopathy. Initial laboratory testing was significant for a WBC of 23,300 (80.2% neutrophils, 13.3% lymphocytes), Hb of 11.1, HCT of 33.1, and ESR of 120. Chest x-ray reported no acute findings and x-ray imaging of affected joints were unremarkable. Blood and urine cultures would eventually return negative. Despite acetaminophen and broad-spectrum antibiotic use, the patient continued with fevers and tachycardia, prompting further infectious and rheumatological work-up. The following all returned negative: HIV, hepatitis, QuantiFERON-Gold, CCP, dsDNA, RF, ANA, COVID-19, typhus IgM/IgG. On hospital day 5, the patient became hypoxic on room air requiring supplemental oxygen. Repeat chest x-ray reported diffuse infiltrates, and CT imaging of the chest reported bilateral ground glass opacities, multifocal pneumonia, and moderate bilateral pleural effusions. Additional testing was negative for repeat COVID-19, two sets of AFB cultures, and for antibodies for Histoplasma, Aspergillus, Brucella, Dengue, Chikungunya, Coccidioides, and Toxoplasma. Monospot testing was positive with negative EBV IgG/IgM and CMV IgM. Only CMV IgG returned positive, nine-fold above the upper limit. The patient would eventually undergo both inguinal and pelvic lymph node biopsies ruling out malignancy during his hospital stay before resolution of fever, tachycardia, and pulmonary symptoms.
Discussion: Cytomegalovirus (CMV) is a prevalent pathogen with 40-100% of the general population showing prior exposure by serology. While primary infection with CMV can often be inapparent, the virus remains latent within the host and is preserved with the ability to reactivate when the host’s immune system is compromised. A common primary presentation consists of a mononucleosis-like syndrome demonstrating acute febrile illness with an increase of 50% or more of lymphocytes or monocytes and at least 10% of the lymphocytes being atypical. Less common presentations of CMV infection include findings such as anemia, exudative pharyngitis, and nonspecific rash, with even rarer presentations including organ-specific complications such as hepatitis, encephalitis, and pneumonitis/pneumonia. As described in this case presentation, the identification of a significant increase in CMV IgG serology with no other likely etiologic agent in the setting of a mononucleosis-like syndrome and significant organ-specific injury suggests CMV as the causative agent. While detection of CMV by PCR in the blood has been identified in prior cases of pneumonitis/pneumonia, few cases have definitely linked CMV as the specific cause in immunocompetent non-transplant patients. As is the situation in this case, the need to further rule out any potentially concomitant undiagnosed immunocompromising conditions is crucial to confirm the etiologic agent as CMV.
Conclusions: In immunocompetent individuals, CMV may be the etiological agent for mild-to-severe febrile illnesses with significant organ-specific dysfunction that requires hospital admission for evaluation and management. Consequentially, additional work-up to identify and rule out undiagnosed immunocompromising conditions in such a situation is vital to establishing the etiologic agent and diagnosis.