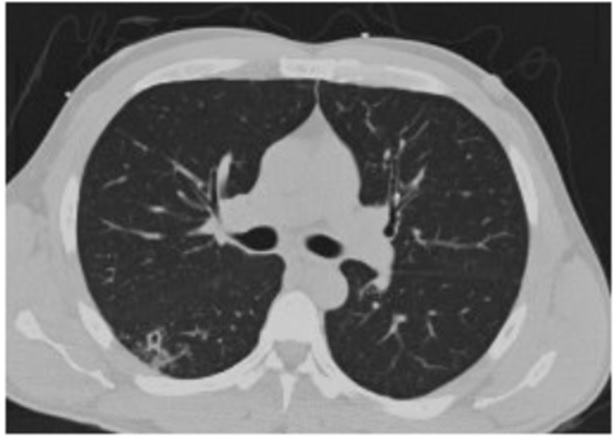
Case Presentation: A 36 year old male from Central America who immigrated to the United States ten years ago presented with cough and headache accompanied with fevers. He did not have any past medical conditions. On admission his vitals were T 39.1 C, HR 114, RR 20, BP 129/85 mmHg. He was noted to have oral thrush and his lungs were clear to auscultation. No neurological deficits were appreciated. Due to the oral thrush he was tested for HIV. His HIV-1 antibodies resulted positive, his absolute CD4 T-cell count was 61 cells/uL and HIV viral load was 36,500 copies/mL. A chest CT revealed nodular infiltrates in the right lower lobe with one of the infiltrates demonstrating a 0.7 cm central cavity. His serum cryptococcal antigen was positive and his blood cultures grew cryptococcus. His TB interferon gamma release assay was negative. He was initiated on amphotericin and flucytosine for disseminated cryptococcal infection with pulmonary involvement. Meanwhile, his lumbar puncture showed 4 total nucleated cells/uL with 25% neutrophils, 65% lymphocytes, CSF glucose was 62 mg/dL and protein was 35 mg/dL, cryptococcal antigen and toxoplasmosis IgG were positive and toxoplasma IgM and AFB smear were negative. Brain MRI with contrast showed a peripherally enhancing 1 cm lesion in the left middle frontal gyrus with mild surrounding vasogenic edema and minimal mass effect.On the discovery of the above ring enhancing lesion there was concern that the patient might have a disseminated cryptococcal infection as well as a concurrent toxoplasma CNS infection, albeit with a singular lesion instead of the commonly seen multiple lesions. Pyrimethamine, sulfadiazine and leucovorin were administered empirically and CSF EBV and toxoplasma PCR testing was sent. However, symptomatically, prior to the initiation of toxoplasma treatment, the patient’s headache had started to resolve and since the lesion was not typical of a toxoplasma CNS infection, further treatment for same was held until confirmatory tests resulted. Eventually, CSF toxoplasma PCR and EBV PCR testing resulted negative and the patient was continued on anti-fungal treatment for disseminated cryptococcal infection with a possible cryptococcoma. In time, CSF cultures demonstrated growth of cryptococcus as well.
Repeat brain MRI with contrast (2 weeks after initiation on antifungal treatment) showed an interval decrease in the size of the previous noted lesion along with a decrease in surrounding vasogenic edema.
Discussion: CNS space occupying lesions in HIV patients are commonly due to toxoplasmosis, EBV associated CNS lymphomas or tuberculomas. This case highlights the presentation of a CNS cryptococcoma, a rare complication of cryptococcal meningitis. In an immunocompromised patient; rejecting Occam’s razor until proven otherwise is a fair practice because multiple opportunistic infections may co-exist in a singular patient. Something to be kept in mind however is that sometimes there can be a singular explanation for an immunocompromised patients myriad of findings but due to the rarity of some of these manifestations we may spend time and effort searching for and treating alternate diagnosis.
Conclusions: The patient’s subsequent lumbar punctures during his hospitalization did not show growth of the fungus. Repeat brain MRI prior to discharge showed a minimal decrease in the size of the lesion and complete resolution of surrounding vasogenic edema. He was discharged home with appropriate treatment to follow-up with Infectious Disease specialists as an out-patient.
.jpg)