Background:
Sepsis is an increasingly frequent problem among hospitalized patients that results in longer lengths of stay and higher mortality. Sepsis is more common among elderly patients and the incidence is expected to rise with aging of the population. There is evidence that early recognition and treatment of severe sepsis including delivery of antibiotics within 1 hour is associated with improved outcomes, but these studies were generally done in ED or ICU settings. Outside these areas, sepsis can be particularly difficult to diagnose because other medical conditions can confuse the clinical picture. Also, most inpatient nursing units are not organized to deliver sepsis care in a 1‐hour time frame.
Purpose:
Code Sepsis is designed to facilitate early recognition of severe sepsis in floor patients and then rapidly deliver a bundle of care based on the Surviving Sepsis Campaign Resuscitation Bundle including drawing a lactate level, obtaining blood cultures before antibiotics, giving antibiotics within 1 hour, and fluid resuscitation in cases with hypotension or high lactate levels.
Description:
All floor patients are monitored for physiologic instability every 8 hours using an aggregate weighted vital sign scoring system. Patients with elevated scores are evaluated by rapid response nurses who screen for sepsis using systemic inflammatory response syndrome (SIRS) criteria and the presence or suspicion of a source of infection. Code Sepsis is activated for all patients who meet these criteria by text paging the first‐call provider, respiratory therapy, the blood gas lab, the pharmacy, and the ICU triage nurse. A Code Sepsis checklist guides care including completion of all bundle elements. The first‐call provider evaluates the patient at the bedside, consults with the attending, and orders the sepsis bundle if indicated. The rapid response nurse draws the appropriate labs and administers IV antibiotics and fluid boluses. Respiratory therapy assists with obtaining arterial blood gases and airway management. The blood gas lab prioritizes Code Sepsis samples and can also perform whole‐blood lactate levels with rapid turnaround times. The pharmacist ensures timely delivery of drugs and assists with antibiotic order entry if the first‐call provider is tied up with intubation or line placement. Finally, the ICU triage nurse locates an ICU bed if the patient requires a higher level of care.
Conclusions:
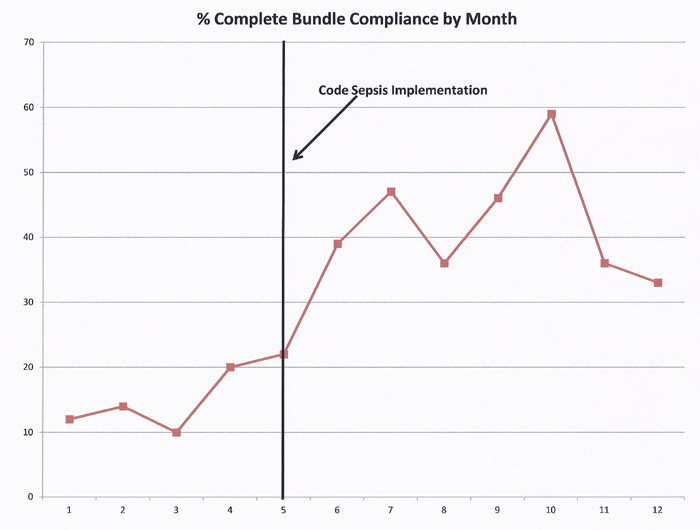
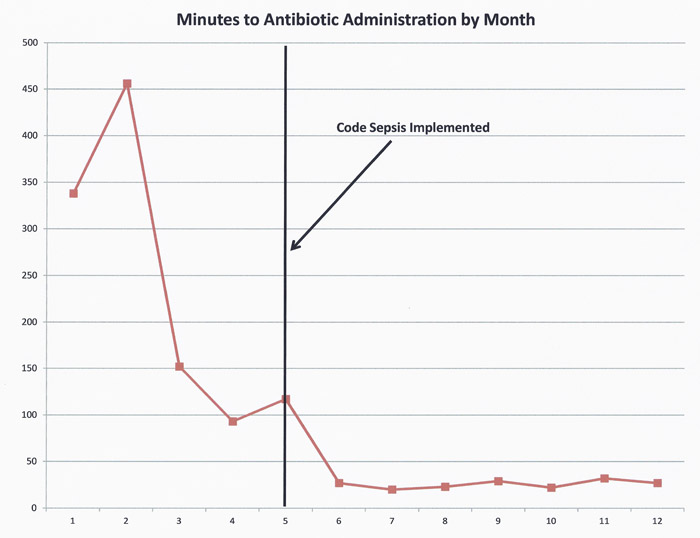
Code Sepsis has resulted in dramatic improvements in process measures for the early recognition and treatment of sepsis in floor patients as shown in the graphs. Risk adjusted mortality and length of stay as calculated by the University Health Consortium have also improved.