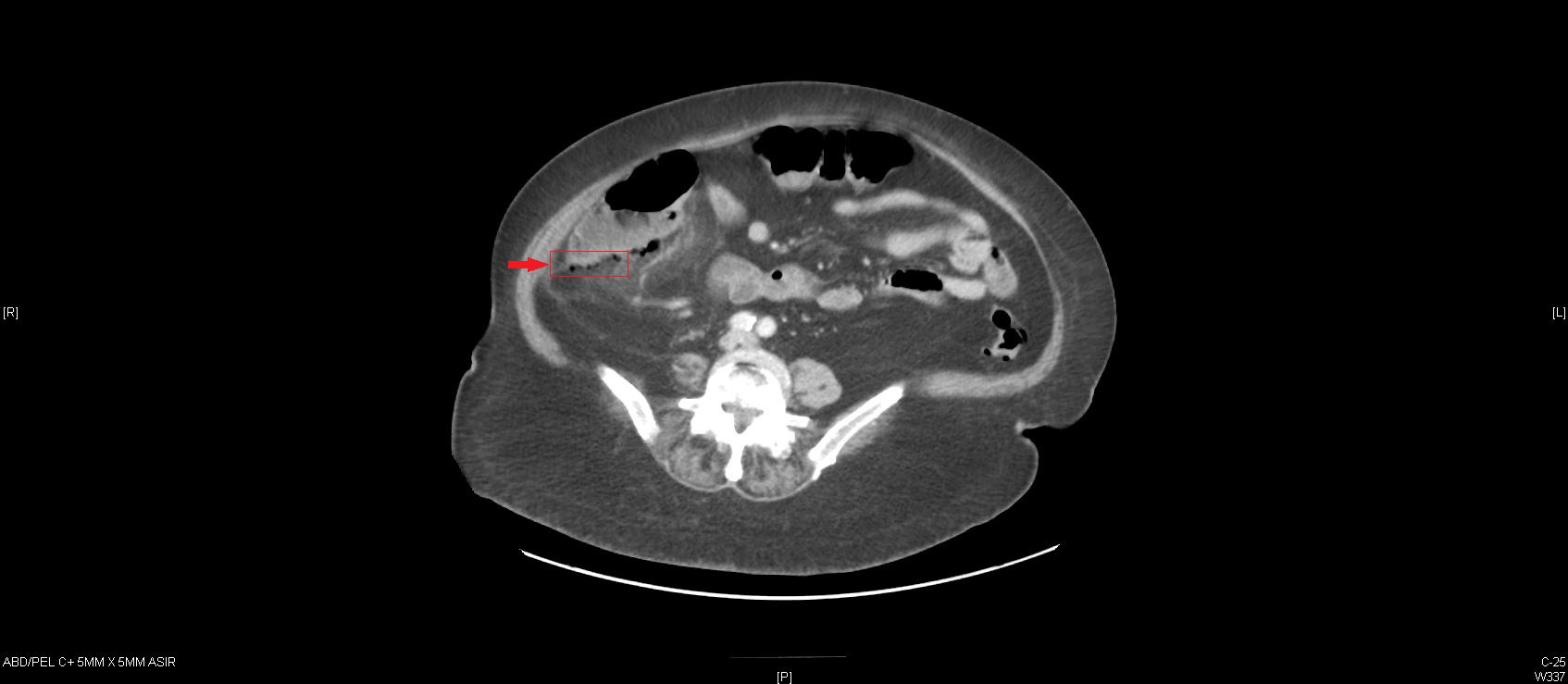
Case Presentation: A 84-year-old woman, with history of diverticulosis and colonic angiodysplasia treated with argon photocoagulation in the past, underwent esophagogastrodudenoscopy (EGD) and colonoscopy for lower gastrointestinal bleeding. She was found to have multiple angiodysplastic lesions in the gastric body, duodenum and proximal transverse colon which were successfully coagulated for hemostasis using argon plasma at 0.3 liters/minute and 30 watts. No biopsy or specimens were collected. Several hours after the procedure, the patient started having abdominal pain.Abdominal exam revealed diffused tenderness, more pronounced in right lower quadrant. Labs were significant for marked leukocytosis of 22,000 cells/mL. She was tachycardic, but afebrile. Empiric antibiotics were started for suspected peritonitis. Plain abdominal radiograph was unremarkable and computed tomography (CT) scan of abdomen showed localized foci of free air adjacent to ascending colon, compatible with colonic microperforation. She underwent urgent exploratory laparotomy and was found to have 2 cm perforation of the posterior wall of cecum distal to ileocecal valve, with no free fluid or gross contamination. Right hemi-colectomy and end-to-end ilicolic anastomosis was performed without any complications. The patient had an uneventful recovery and was discharged home on postoperative day 5.
Discussion: Colonic microperforation (CP) is a rare but serious complication of colonoscopy, resulting in high morbidity and mortality. It occurs as a result of tractional forces against the bowel wall, barotrauma or as direct result of therapeutic interventions during colonoscopy. Sigmoid colon is the most common site, but cecal involvement particular in elderly patients due to thinning of cecal wall with age. The frequency of CP is an estimated 0.3-3%, with higher rates attributed to therapeutic colonoscopies. Advanced age, female gender, and underlying diverticular disease are some factors contributing to higher rates of CP after colonoscopy. Diagnosis may be established by plain film radiography, however abdomen CT is superior and necessary in cases of unrevealing X-ray. Optimal management of CP, whether conservative or surgical, remains controversial. Our patient underwent aggressive surgical treatment in view of sepsis and advanced age, however there was no evidence of peritonitis on during exploration.
Conclusions: CP should be suspected in all patients with acute onset abdominal pain after colonoscopy. We recommend obtaining CT scan of abdomen for all patients with high suspicion of CP who had colonoscopy as plain films may not be diagnostic always. Management should involve multidisciplinary approach including surgeons, radiologist and gastroenterologist, that can individualize patients for conservative or surgical approach based on their clinical severity and underlying co-morbidities.