Background: The U.S. healthcare system has a poor safety record when compared to other major industries. For example, at 250,000 per year, medical errors are the 3rd leading cause of death according to the CDC. This is in stark contrast to the safety record of commercial jet airlines. With zero fatalities, fiscal year 2017 was the safest in commercial airline industry history. Experts in airline safety believe this is primarily due to the adoption of stringent quality improvement (QI) methods that continuously identify and assess potential safety threats in order to optimize protective safety barriers that prevent or mitigate harm. A common method used to assess risk and optimize protective barriers is Bow-Tie analysis.
Purpose: In our current study we describe the use of Bow-Tie analysis, combined with standard lean six-sigma methodologies, to develop interventions to reduce hospital-acquired venous thromboembolism (HA-VTE).
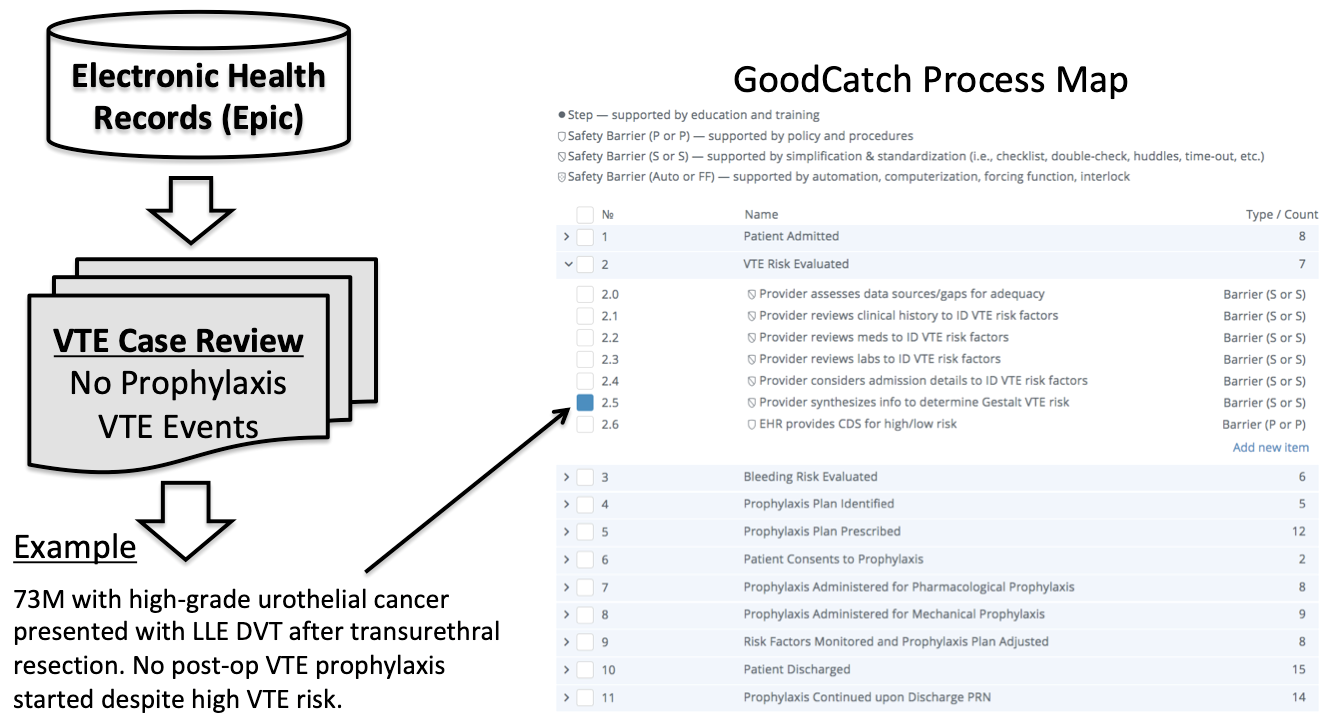
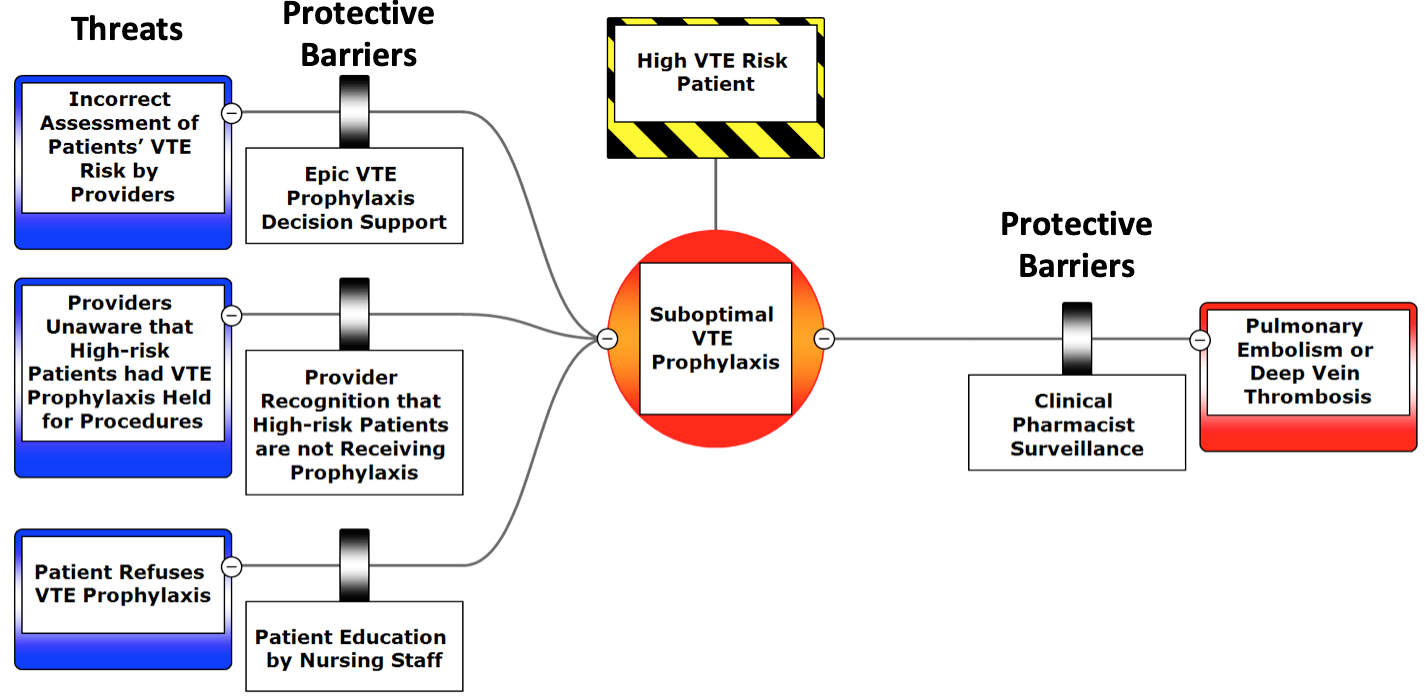
Description: Using electronic health record data to identify patients with acute HA-VTE events and high-risk patients not on VTE prophylaxis, all failures in processes of care were recorded and analyzed using process map software over a 3-month period (figure 1). The results of the analysis were summarized using Bow-Tie risk analysis (figure 2). The analysis showed the following threats to optimal VTE prophylaxis: 1) incorrect assessment of patients’ VTE risk by providers, 2) providers being unaware that high-risk patients had VTE prophylaxis held for surgical procedures, and 3) patient refusal of VTE prophylaxis. We identified the following protective safety barriers: 1) Epic decision support for VTE prophylaxis, 2) provider recognition of high-risk patients not on prophylaxis, 3) patient education on importance of VTE prophylaxis, and 4) clinical pharmacy surveillance of VTE prophylaxis. All protective safety barriers were determined by the workgroup to perform sub-optimally.
Conclusions: Based on the analysis, our institution is implementing the following interventions: 1) upgrading Epic VTE decision support to reflect evidence-based guidelines, 2) standardizing clinical pharmacy workflow to improve surveillance of VTE prophylaxis, and 3) standardizing scripts for nurses to educate patients refusing VTE prophylaxis. In conclusion, we were able to combine QI methodologies used by other industries, specifically Bow-Tie analysis, with lean six-sigma to develop interventions to reduce HA-VTEs. Bow-Tie analysis potentially offers a formalized method to assess process failures and design interventions to improve the quality of patient care.