Background: Daily lab (DL) overuse in hospitalized patients leads to increased costs and resource utilization, iatrogenic anemia, and patient discomfort. Those awaiting discharge to post-acute care, who experience frequent non-medical delays in discharge, may represent an important group of patients at risk of receiving unnecessary DL, especially labs on day of discharge (LOD). Best Practice Alerts (BPAs) on electronic health records (EHRs) can reduce lab testing, with some evidence showing a sustainable reduction in lab ordering practices.
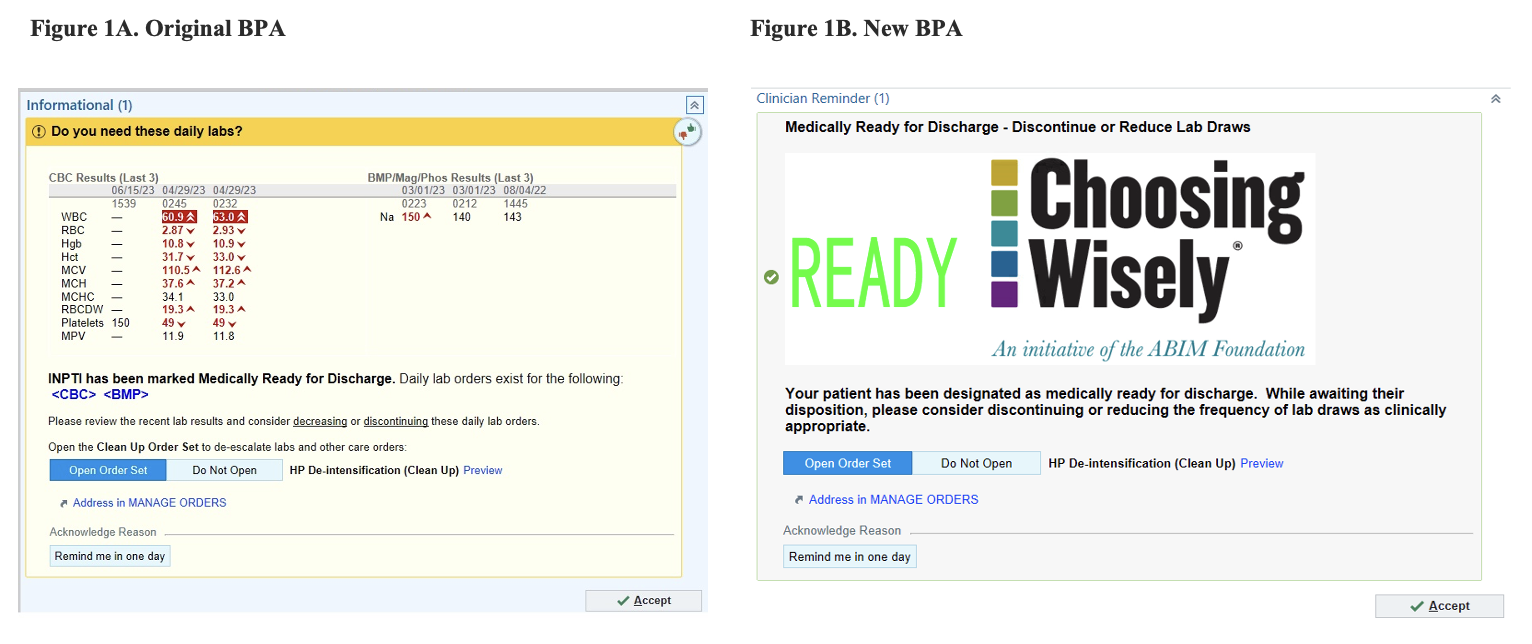
Purpose: This study aimed to reduce DL and LOD for patients who were medically ready for discharge through implementation of a BPA on multiple hospital services. The BPA was designed iteratively by quality experts to compare the prevalence of DL and LOD between the original BPA versus the re-designed BPA. The color and heading of the new BPA were switched from yellow to grey and from “Do you need these daily labs?” to “Medically Ready for Discharge – Discontinue or Reduce Lab Draws,” respectively. It also includes a large “Choosing Wisely” logo and has the same options as the original BPA. The options include opening a “De-intensification (Clean Up)” order set in which a provider could choose to space labs, addressing lab-ordering in the “Manage Orders” tab, or clicking a “Remind me in one day” button. The purpose of this study was to assess if using a clearer heading, changing the color of the BPA to one that is not used as frequently, and using a logo would minimize alarm fatigue and encourage providers to open the order set within the BPA.
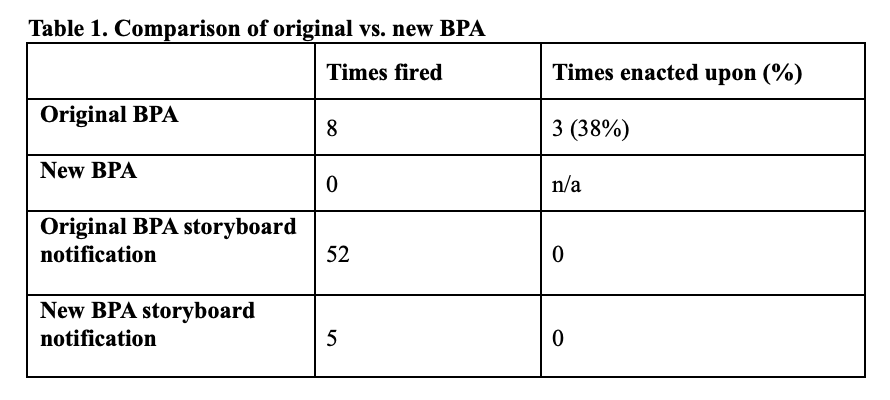
Description: This study was conducted at an academic tertiary medical center on 2 direct care hospitalist-PGY3 resident services and 1 short stay unit (SSU) service staffed by advanced practice providers (APPs). During multidisciplinary rounds, the primary service (attending, PGY3, or APP) designated medically ready patients to the social worker, who clicked a “Medically Ready” button in the EHR. A BPA then fired as a pop-up in the “Manage Orders” tab stating the patient was medically ready and/or as a “Medically Ready” alert on the sidebar or storyboard of the patient’s chart. When clicked, it guided the provider to the lab-ordering section. The original BPA went into effect in March 2023. The new BPA was launched November 1. Data were retrospectively extracted to determine how many times the BPA fired and if it was dismissed or acted upon for each encounter. The BPA was considered enacted upon if the provider opened the “De-intensification” order set or clicked on “Address in Manage Orders” in the BPA.Since March, the original BPA fired 52 times in the storyboard and was enacted upon 0 times. The BPA fired 8 times as a pop-up in the “Manage Orders” tab and was enacted upon 3 times (38%). The new BPA fired 5 times in the storyboard and was enacted upon 0 times. It has not yet fired as a pop-up in the “Manage Orders” tab.
Conclusions: Provider interaction with the pop-up BPA was more likely than with the storyboard BPA. Thus far, this study suggests that providers respond more to a pop-up BPA and may accomplish greater change than an alert in the storyboard. However, given that the new BPA has only been implemented for 4 weeks, there are limited data to compare the old design with the new one. Collecting more lab-ordering data with the newly designed BPA and expanding the BPA to other services may demonstrate an overall reduction in DL and LOD for medically ready patients. Regardless, optimizing integration with workflow is important to creating change and ensuring appropriate patient care.