Background: Care coordination during the patient’s hospitalization is one of the most important goals to achieve as it affects quality and efficiency outcomes, including length of stay. Multidisciplinary Rounds (MDR) aim to discuss each patient’s care plan in every unit. In our inner-city safety net hospital, each inpatient unit conducted MDR differently. The MDRs varied in participating disciplines, the content discussed, and their goal. In particular, the MDRs needed more consistent discussion about the Expected Date of Discharge (EDD), which would have allowed the team to coordinate the discharge starting the day of admission. Thus, siloed work by MDR members caused avoidable length of stay.
Purpose: A discharge efficiency work group was conducted to standardize MDRs with scripted content and clear roles and responsibilities. The providers were tasked to report EDD on every patient and take the necessary steps to achieve the EDD. The EDD reporting rate and average monthly Length of Stay (LOS) were measured to analyze the impact of the standardized MDRs
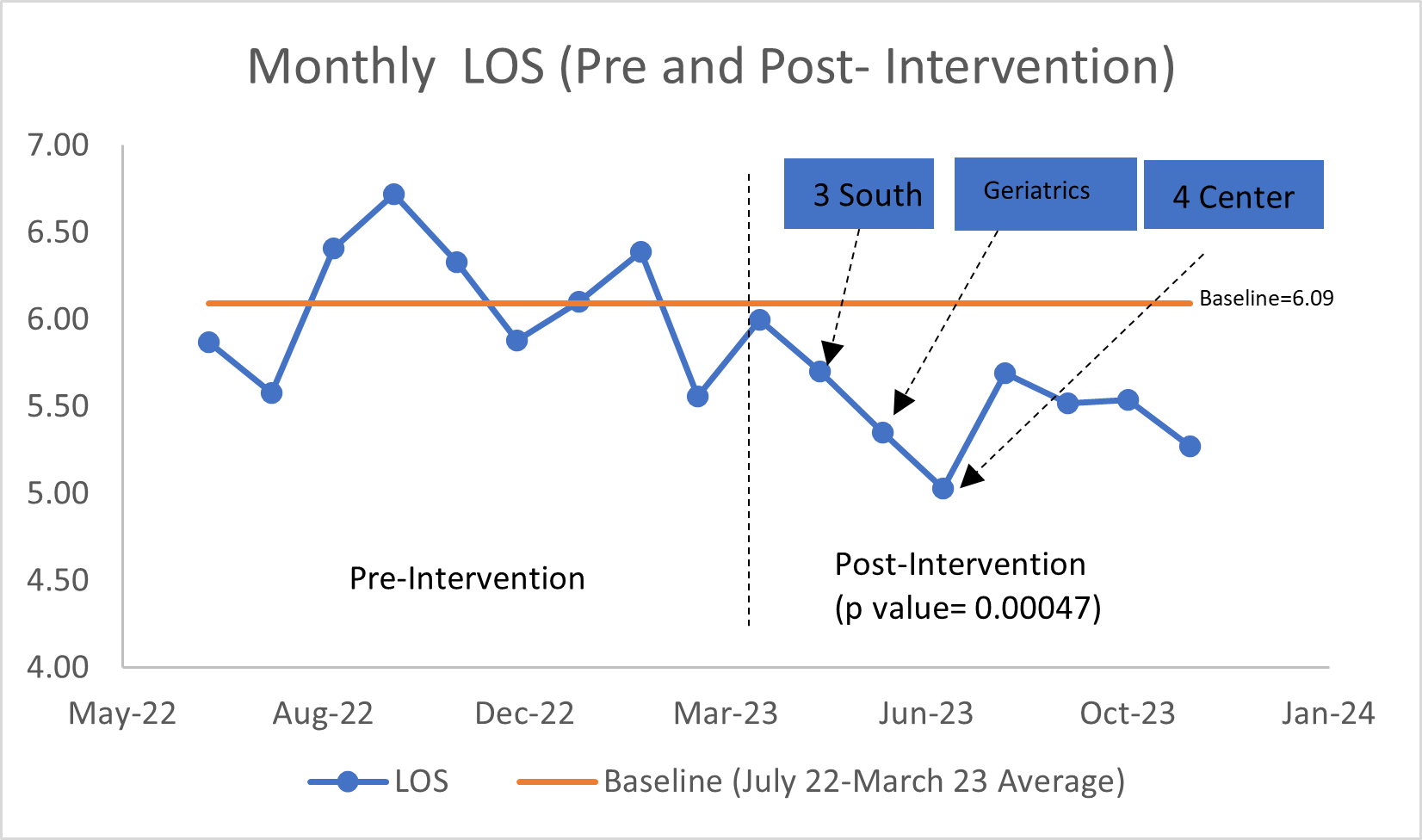
Description: The discharge efficiency work group consisted of hospitalists, RNs, Case Managers, Social Workers, pharmacists, and Physical Therapists who worked on standardizing the MDRs. The main goal for MDR was to coordinate the care for each patient and target to get the patient ready for discharge based on reported EDD by the providers. The standardized MDR project was first implemented on the largest medical unit in the hospital in April 2023. Case Managers led the pilot unit MDR. The attending provider is the first team member to present the patient’s active medical issues and EDD. The attending provider was tasked with reporting EDD for every patient and documenting or updating it in EMR after the MDR. The Nurse, Case Manager, Social Worker, Pharmacist, and Physical Therapist followed the provider’s presentation in the same order for every patient. The Case Manager for the unit would summarize the discharges for that day and the following day at the end, based on the discussion at MDR.This process was audited by the quality management team twice a week. The study process measures were the rate of EDD discussion and the rate of EDD documentation on Electronic Medical Records. The outcome measure was the monthly average Length of Stay. The standardized MDR was scaled up to other inpatient units between May and June 2023.Results:The average LOS during the pre-intervention period (July 2022- March 2023) was 6.09 with a standard deviation of 0.4. The post-intervention period (April- November 2023) average LOS was 5.51 with a standard deviation of 0.3. The difference between the pre-intervention and post-intervention length of stay was statistically significant with a p value of 0.00048 using two population t-statistics test.The standardized MDR intervention also showed a 4-fold improvement in EDD discussion and documentation rate, as evidenced by the weekly audit data (see bar graph below).
Conclusions: Our standardized MDR intervention demonstrates that early discussion and documentation of Expected Discharge Date on hospitalized patients during multidisciplinary rounds results in a sustained reduction in Length of Stay through timely initiation of discharge planning and other services through members of the patient care team. This project has since been scaled up to the other units in the hospital.