Background: Sickle cell disease (SCD) and its vasoocclusive sequela are significant causes of morbidity and mortality as well as acute care utilization throughout the United States, with an estimated 92,880 hospital admissions totaling $759 million in aggregate annual costs in 2014. There is a need within health care systems to identify strategies for achieving higher value care for this patient population. In recent years, hospitalists have taken on a larger role in the care for this patient population in comparison to hematology specialists in more traditional delivery models. We sought to compare the outcomes for patients cared for by these unique provider groups over recent years at our institution.
Methods: We performed a retrospective analysis of patients hospitalized for sickle cell disease related complications (using ICD 9 or 10 coded diagnoses) from September 2009 – December 2017. Financial data from these encounters pertaining to patient demographics, cost/charges, length of stay, and readmission was analyzed to compare baseline characteristics and outcomes for patients under the primary care of hospitalists against those under the primary care of hematology specialists. Outcomes were adjusted with regression modeling. The two-sample t-test was utilized to compare the distributions of major outcomes with continuous variables and the chi-square test was used for categorical variables.
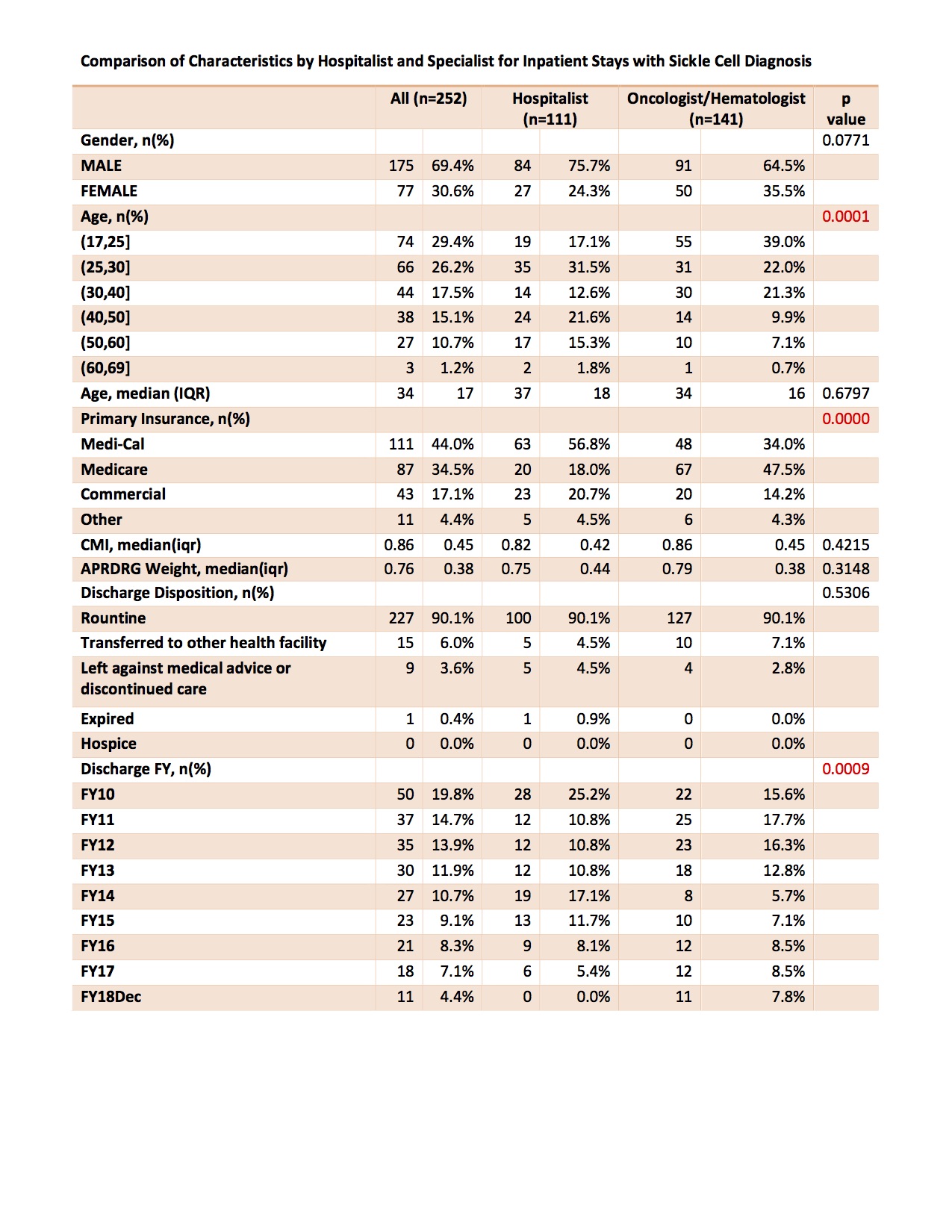
Results: From September 2009 – December 2017 there were 252 inpatient admission encounters for adults with a sickle cell disease related complication. Patient characteristics for these encounters are shown in FIgure 1. The case mortality index for both groups was comparable (0.86 vs. 0.82) as was the proportion of patients who left against medical advice (4.5% vs. 2.8%). Comparison between hospitalist and hematologist patient outcomes failed to reveal a statistically significant difference in length of stay or 30-day readmission between groups. Hospitalist admissions resulted in significantly lower total direct costs (65% of average hematology admission charges, 95% CI 47.5% – 89.7%) and transfusion direct costs (61.6%, 95% CI 44.9% – 85.0%).
Conclusions: In our study, there were significantly lower total direct costs and transfusion direct costs for patients hospitalized under the care of hospitalists when compared to hematologists. There was not, however, a significant difference in average length of stay or readmission rate. We observed average length of stay and 30-day readmission rates comparable to those reported in the Healthcare Cost and Utilization Project Database.
Our study has several limitations. First, this is a retrospective observational study, in which unobserved variables may bias results. Second, this is a single center study performed at an academic medical center, for which results may not be generalizable to alternative practice settings. Third, we have relied on administrative financial data for this analysis, which is subject to potential recording errors. Fourth, our limited sample size diminishes the power of our analysis and may hinder interpretation of results.
In conclusion, we noted reduced total and transfusion direct costs for patients with sickle cell disease cared for by hospitalists while also demonstrating no significant difference in average length of stay or the 30-day hospital readmission rate. Further investigation is warranted in order to identify systems based mechanisms for promoting lower cost, higher quality care for this vulnerable patient population.