Background: As generalist physicians on the frontlines of hospital care for seriously ill patients across the country, hospitalists are optimally positioned to lead discussions regarding serious illness. Little is known about hospitalists’ confidence in serious illness communication, or the barriers that limit their engagement.
Methods: To assess perspectives on serious illness communication, we surveyed hospitalists at two urban academic medical centers in Spring 2015. The survey was developed by the authors based on published research, discussions with colleagues, and clinical experience. The final survey included Likert-type questions assessing hospitalists’ confidence to perform 14 serious illness communication tasks, and the degree to which 12 potential barriers were concerns when communicating with seriously ill patients and their families. All attending hospitalists at each institution received an email invitation with a link to complete the online survey. Differences in responses between institutions were assessed with Fisher’s exact and Chi-square tests.
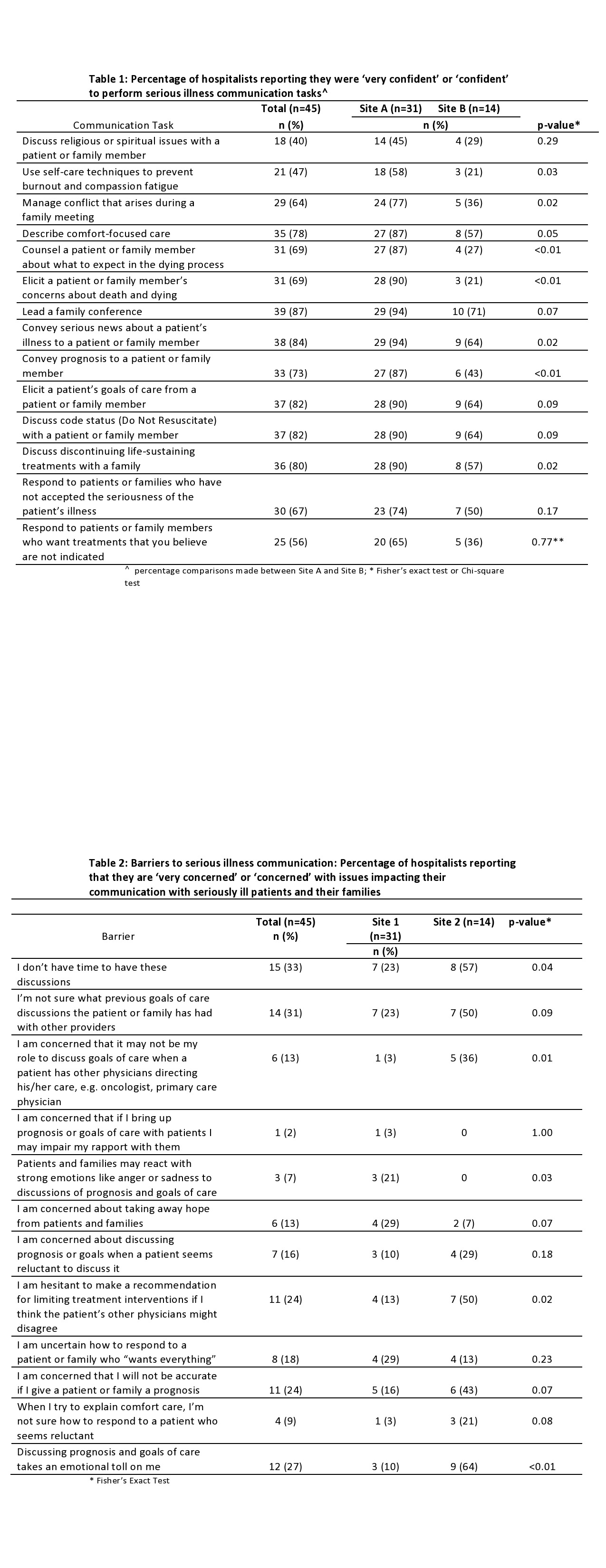
Results: A total of 45 hospitalists completed the survey; response rates were 43% at Hospital A and 46% at Hospital B. Participants reported the highest levels of confidence for leading a family meeting and eliciting goals of care, and the lowest confidence for discussing religious or spiritual issues, performing self-care to prevent burnout and compassion fatigue, and responding to desire for interventions that are not medically indicated. Confidence was higher at Hospital A for 13 of the 14 tasks (Table 1). Issues posing greatest concern in discussing serious illness with patients and families were time constraints, lack of knowledge of patients’ prior conversations, and the emotional toll these conversations take on the hospitalists; the areas of greatest concern varied by hospital (Table 2).
Conclusions: Efforts to engage and support hospitalists in serious illness communication should focus on complex communication tasks such as discussing religious beliefs and managing conflict. Promotion of and support for self-care is also an area of great need for hospitalists engaged in these conversations. Future work should focus on further characterizing differences in confidence and barriers across institutions, and identifying factors that predict these.