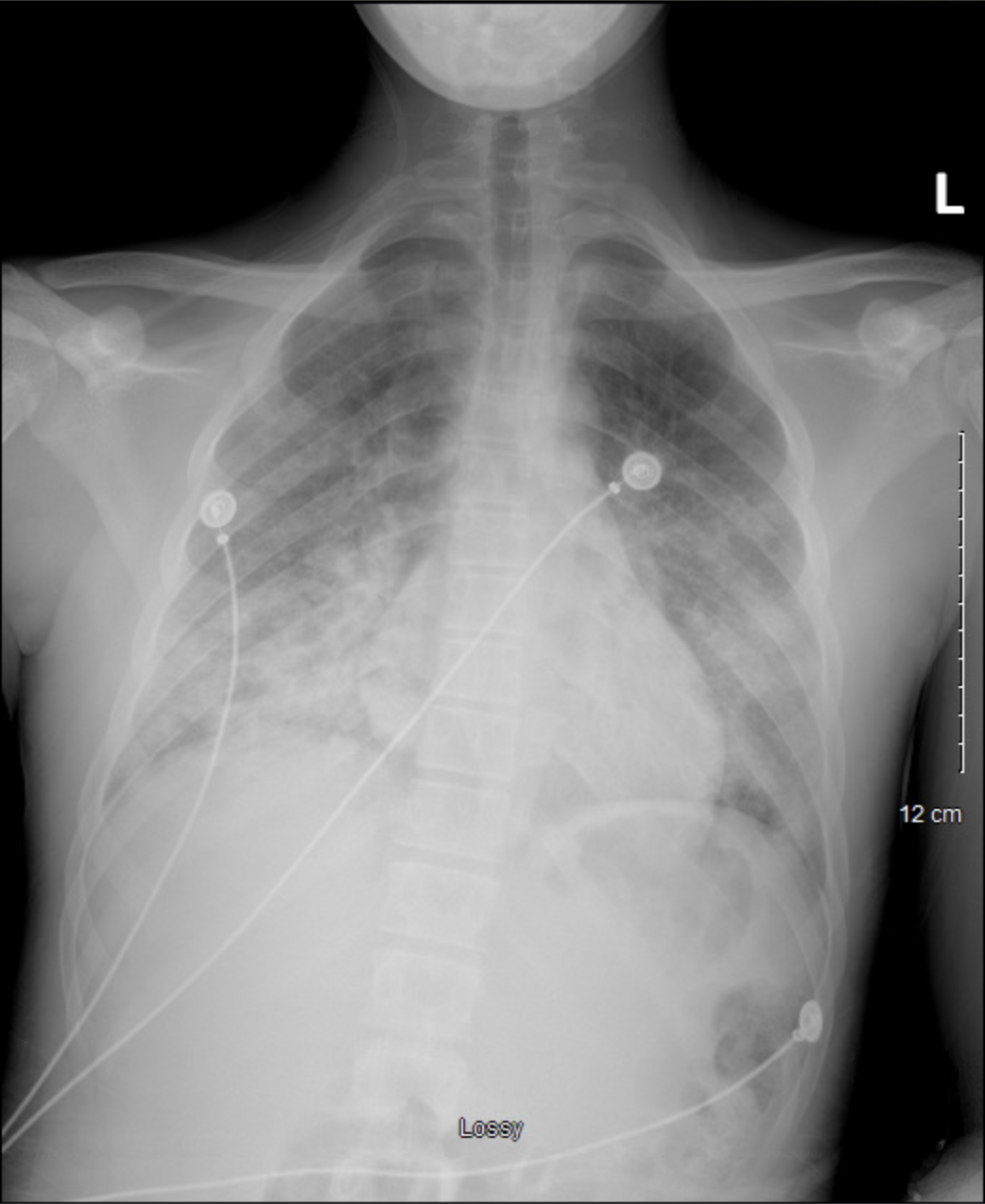
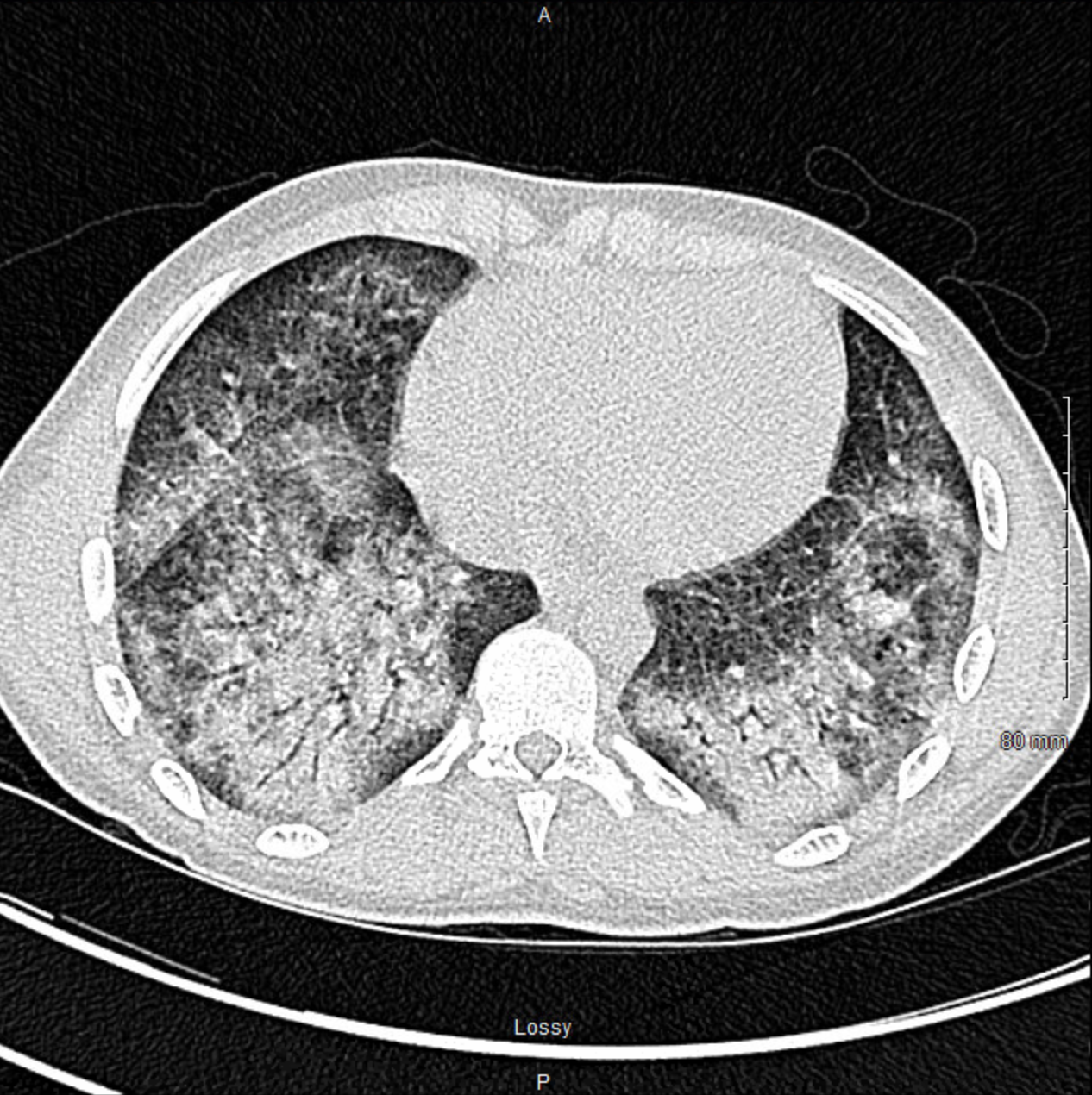
Case Presentation: A 17-year-old male presented with 4 days of shortness of breath, fatigue, tachypnea, chest pain, diffuse abdominal pain, and poor appetite. Labs notable for a negative COVID PCR,WBC 17, ferritin 938, lactic acid 2.2, LDH 613, CRP 40.3, procalcitonin 1.08, and THC positive. Multisystem Inflammatory Syndrome in Children (MIS-C) workup resulted negative COVID IgM/IgG, troponin normal, initial BNP 51 rising to 1,350, IL-6 88.4, D-dimer 2,402, fibrinogen > 1,000, and PT 17.9 Blood culture, sputum culture, and respiratory pathogen panel were negative. Imaging included CXR with extensive bilateral perihilar infiltrates (Figure 1) and CT showed patchy regions of ground-glass opacification throughout lungs with a peripheral and lower lung predominance (Figure 2). Findings were concerning for MIS-C and patient was started on IV methylprednisolone, enoxaparin, and empiric antibiotics.Patient required supplemental oxygen to maintain saturation and required high-flow nasal cannula during PICU admission. He was able to wean to room air on day 5 of admission.Pulmonary function tests (PFTs) prior to discharge showed FEV1 67(71), FVC 65(69), FEV1/FVC 90(89), and FEF 25-75 61(98), suggestive of mixed restrictive/obstructive defect with significant improvement in flow of the small airways following bronchodilator. Upon further investigation into social history, patient revealed that he heavily used vape products over the last year with almost daily use of THC vaping products. Once stable on room air and abdominal pain was controlled, patient was discharged on a PO steroid taper and enoxaparin. His primary diagnosis was E-cigarette or Vaping Product-Use Associated Lung Injury (EVALI). Four weeks later, he no longer had dyspnea or respiratory distress. He did endorse brief, intermittent episodes of chest tightness. Follow-up PFTs were: FEV1 93(93), FVC 92(89), FEV1/FVC 88(91), and FEF 25-75 93(105). The patient was strongly counseled on avoidance of vaping and other inhalants including marijuana use.
Discussion: The majority of patients with EVALI (52%) have been younger than 24 years old [1]. In an analysis of pediatric EVALI, gastrointestinal and constitutional symptoms were present in all 11 patients whereas shortness of breath and cough were reported in 5/11 and 6/11 patients, respectively [2]. A targeted, detailed vaping history in an adolescent with either respiratory or gastrointestinal complaints is becoming an important part of the diagnostic work-up in the hospital setting. A basilar-predominant consolidation and ground-glass opacity on CT has been associated with this entity [3]. If this pattern is identified on chest CT in a patient with any vaping history, EVALI should be strongly considered. Diagnosis is based on: 1) E-cigarette or vaping product use within 90 days of symptom onset, 2) Pulmonary infiltrate on CXR or chest CT, 3) Absence of pulmonary infection on work-up, and 4) no evidence in the medical record of alternative plausible diagnoses [4]. A definitive diagnosis may be made if vitamin E acetate is identified in bronchoalveolar lavage fluid [5], but this may not be practical in the era of COVID-19.
Conclusions: EVALI is a disease entity that has become more prevalent in recent years. Due to its nonspecific symptomology and overlapping imaging findings with the COVID-19 virus, it is important for clinicians to maintain a high index of suspicion while still ruling out all other possible diagnoses. Overall, prompt recognition and preventative education of adolescents should be emphasized.