Background: Recent research highlights that in-hospital communication increasingly is relying on secure electronic messaging with notable unintended consequences, including increasing task switching and the overall burden of communications. This study sought to quantify non-actionable, non-urgent messages to better understand their prevalence and to develop interventions aimed at optimizing communication workflows.
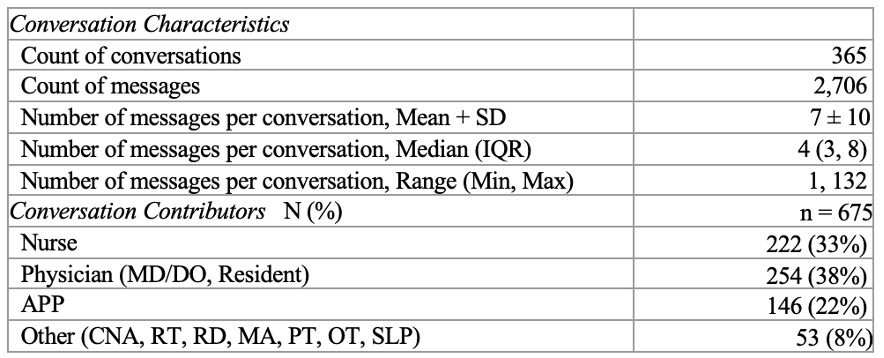
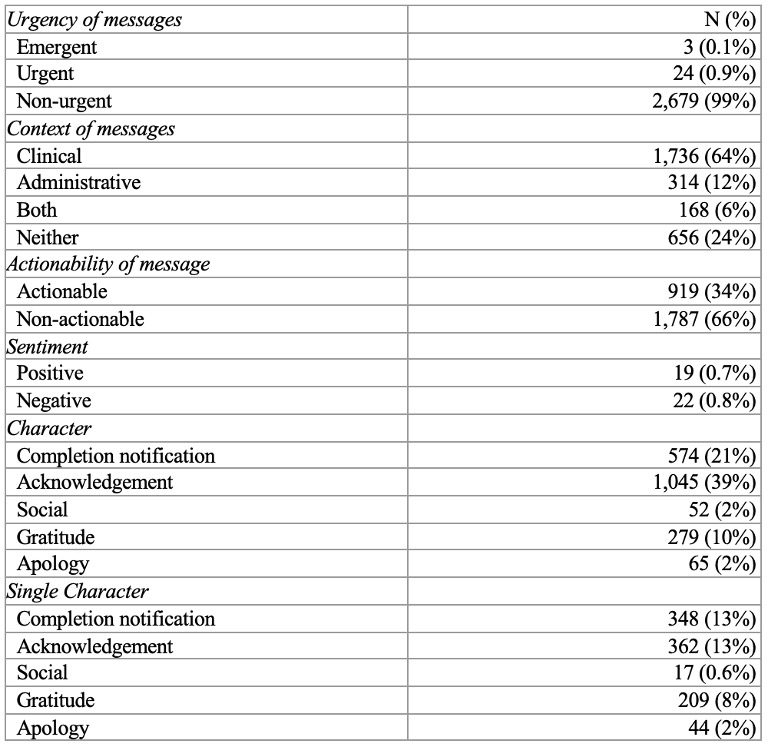
Methods: A qualitative content analysis was performed on a randomly selected subset of messages sent and received by hospitalist clinicians from a weekday and a weekend day during 2023, coding them by urgency (i.e., emergent, urgent, non-urgent), context (i.e., clinical, administrative), actionable/non-actionable, content (i.e., social, gratitude, acknowledgement, apology, completion notification), sentiment (i.e., positive, negative, neutral), and other key features (i.e., change in communication mode, near miss/miss, presence of emoticon). A thematic analysis was then conducted on conversations that were length outliers (i.e., greater than one standard deviation) or contained messages with emotion, messages indicating a change in communication mode, and messages highlighting a near miss/miss event.
Results: A total of 2706 messages (365 conversations) were coded by the study team. These messages were sent and received by physicians (38%), advanced practice providers (22%), nurses (33%), and other care team members (8%). The majority of these messages were “non-urgent” (99%), “clinical” (64%), and/or “non-actionable” (66%). Among these messages, many were characterized as solely acknowledgement (13%), completion notification (13%), gratitude (8%), or acknowledgement and gratitude (8%) with a smaller subset of messages containing only components of social interactions (0.6%) or apology (2%). Conversations that were length outliers (19%) typically involved discussions of complex and evolving patient-related topics. Themes for conversations containing a near miss/miss event (7%) included a lack of knowledge or information related to a care plan, order errors, messaging the wrong person or regarding the wrong patient, failure to complete an action item, and failure to communicate important patient events. Communication mode changes (5%) typically involved transitions to phone call for further discussions (e.g., updates, questions) and to facilitate in-hospital transfers of care, as well as transitions to in-person conversations for clinical status changes and to email for sending attachments. Emotions (29%) were conveyed in conversations through language, capitalization and punctuation, and emoticons.
Conclusions: A majority of messages were non-urgent and non-actionable with many containing lower acuity elements, specifically acknowledgement, gratitude, or completion notification. These messages may offer a specific target for addressing communication volume and related interruptions.