Background:
The diagnosis of acute cholecyslitis is usually straightforward, but determining whether common bile duct (CBD) stones are present is usually not. Clinicians rely on clues such as a dilated CBD, intrahepatic ductal dilation, elevated bilirubin and/or alkaline phosphatase, and jaundice to estimate the likelihood of CBD stones in patients with acute cholecystitis, Clinicians must also choose a treatment strategy without knowing for certain whether CBD stones are present. Both endoscopic retrograde cholangiopancreatography (ERCP) with sphincterotomy and laparoscopic common bile duct exploration (CBDE) are safe and reliable methods of clearing stones from the CBD. Because these 2 strategies are equally efficacious, our aim was to determine which is the most cost effective.
Methods:
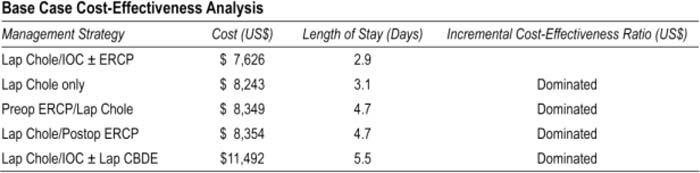
We did a cost‐effectiveness analysis and built a decision model including 5 possible strategies for treating patients with acute cholecystitis and possible CBD stones: (1) laparoscopic cholecystectomy (lap chole) only, (2) preoperative ERCP followed by lap chole, (3) lap chole with intraoperative choiangiography (IOC) + CBDE if CBD stones are detected during IOC, (4) lap chole followed by postoperative ERCP, and (5) lap chole with IOC + postoperative ERCP if CBD stones are detected during IOC, The probabilities of cannulating the CBD, CBD stone removal, morbidity, and mortality associated with lap chole ± CBDE and ERCP and the sensitivity and specificity of IOC and ERCP were acquired from published literature and used in the model. The cost of hospitalization was from the 2006 National Centers for Medicare and Medicaid data, Professional fees for each procedure were determined using Current Procedural Terminology codes. Each strategy was modeled until either the patient died, was found to not have CBD stones, or was found to have CBD stones and then underwent removal. The target population is patients with acute cholecystitis and possible CBD stones, The base case scenario was a 30‐year‐old woman who develops acute cholecystitis and has a 10% likelihood of CBD stones. The likelihood of CBD stones was varied from 0% to 100% and the most cost‐effective strategy for each likelihood was determined.
Results:
If the likelihood of CBD stones is 5%–90%, the most cost‐effective strategy is lap chole with IOC ± postoperative ERCP, If the likelihood is less than 5%, the lap chole only strategy is cost effective. If the likelihood is 90%–1O0%, the preoperative ERCP and postoperative ERCP strategies are cost effective. Our model was only sensitive to 3 costs, the cost of hospitalization for lap chole with CBDE, the cost of hospitalization for lap chole without CBDE, and the cost of lap chole with IOC.
Conclusions:
The most cost‐effective treatment strategy for the majority of patients with acute cholecystitis is lap chole with IOC with postoperative ERCP if stones are detected on IOC, Cost‐effectiveness analyses are useful for comparing the relative costs and outcomes of several possible treatment strategies.
Author Disclosure:
L. Brown, none; S. Rogers, none; J. Cello, none; J. Inadomi, none.