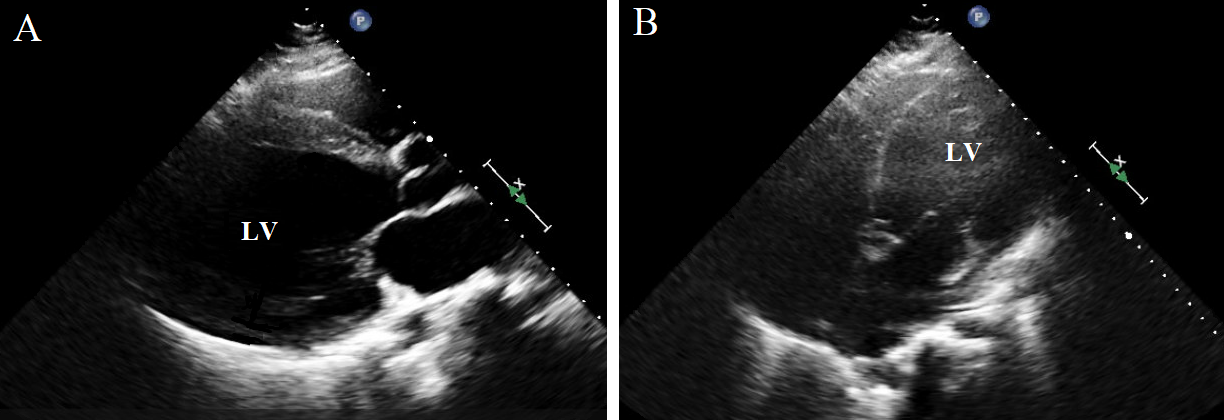
Case Presentation: A 31-year-old male with a past medical history of dilated cardiomyopathy (ejection fraction 20%) presented with shortness of breath. Initial blood pressure was 83/53 mmHg. His breathing became agonal and therefore he was intubated. Physical examination demonstrated jugular venous distention and cold extremities. Chest radiography (Figure 1) revealed diffuse and complete opacification of the right lung. An echocardiogram (Figure 2) revealed an ejection fraction of 10%. He was diagnosed with cardiogenic shock and started on dobutamine and norepinephrine. Intravenous epinephrine was added later on. Furosemide was administered, however he remained persistently hypotensive and oliguric, and therefore he was started on milrinone and vasopressin as well. Nasopharyngeal swab for SARS-CoV-2 was positive. His urine output continued to decline and was eventually started on continuous veno-venous hemofiltration. Overall, his shock state was thought to be mixed; cardiogenic and vasodilatory, in the setting of COVID-19. Unfortunately, the patient expired several days later.
Discussion: In December 2019, a cluster of cases of pneumonia were identified in China that was attributed to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The published data so far regarding Coronavirus Disease 2019 (COVID-19) have identified that cardiovascular complications mainly manifest as myocardial injury, heart failure, acute coronary syndrome (ACS) and arrhythmias.Potential mechanisms for cardiovascular involvement include systemic inflammation, demand ischemia and pathogen-mediated damage. Infection with SARS-CoV-2 results in the release of pro-inflammatory cytokines including interleukin-6 which may lead to endothelial cell damage as well as left ventricular remodeling and systolic dysfunction.Myocardial injury is mainly due to hypoxia especially in the setting of acute respiratory distress syndrome (ARDS). Severe COVID-19 may eventually lead to ARDS manifesting as hypoxemia with ground-glass opacities on chest radiography, however similar findings have been reported as well with coexisting cardiogenic pulmonary edema. Since ARDS and sepsis share similar underlying mechanisms, characterized by endothelial dysfunction, it is important to recognize the coexistence of both cardiogenic and vasodilatory components of shock state in COVID-19. ACS secondary to COVID-19 is multifactorial in etiology including virally-induced systemic inflammation and elevated thrombotic state. Another manifestation of COVID-19 is arrhythmias which are mainly attributed to the significant hypoxia and neuro-hormonal stress.Various pharmacologic agents being used for COVID-19 are associated with potential cardiovascular complications. Chloroquine and hydroxychloroquine have the potential for intermediate-to-delayed myocardial toxicity as well as prolongation of the QT interval and therefore an increased risk of torsades de pointes. Regarding antiviral therapy, a number of agents are under investigation including lopinavir/ritonavir and remdesivir. Lopinavir/ritonavir may result in QT interval prolongation, and cardiovascular toxicity from remdesivir is yet to be reported.
Conclusions: In light of the emerging pandemic of COVID-19, several cardiovascular complications of the infection itself or the proposed therapies are gaining worldwide recognition. Awareness of such entities is required for early recognition to prevent grave sequelae.