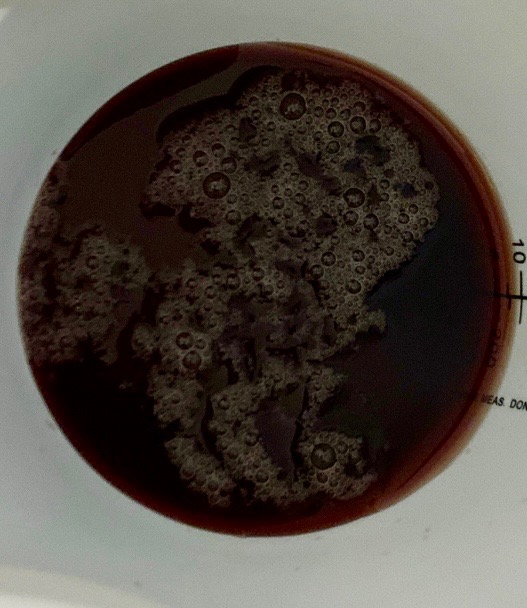
Case Presentation: This is a 4-year-old previously healthy girl, fully immunized with the exception of COVID-19 immunizations, who was hospitalized after presenting with fevers and fatigue for one week followed by gross hematuria. At the outset of her fevers, she tested negative for COVID-19 using a home antigen test. 4 days prior to admission, she tested positive for COVID-19 and began to experience gross hematuria. Review of systems was notable for lack of significant respiratory symptoms, changes in appetite, abdominal pain, nausea, vomiting, dysuria. In the emergency department, she was noted to have frank hematuria (figure 1). Physical examination showed her to be normotensve and febrile. With the exception of mild jaundice and icterus, the remainder of her exam was unremarkable. Urinalysis was significant for dark red/brownish color, 2+ albumin, 3+ hemoglobin, trace leukocyte esterase, 20 WBCs/hpf, 3 RBCs/hpf. CBC abnormalities included Hb 8.4 g/dL, Plt 94 k/mm3. Serum chemistries were significant for Cr 0.5 mg/dL, BUN 23 mg/dL, total bilirubin 6.0 mg/dL. She was admitted and subsequently her Hb dropped to 6.9, requiring a PRBC transfusion. Hematology/oncology was consulted, and subsequent workup revealed a borderline low C3 at 84 mg/dL, normal C4 of 12 mg/dL and haptoglobin < 10 mg/dL. Coombs testing showed positive anti-C3d and negative anti-IgG, consistent with cold agglutinin disease. D-dimer was elevated at >35.20 ml/L, and INR, PT, PTT, fibrinogen were normal. Peripheral smear showed no evidence of schistocytes. Throat culture was negative for Group A Strep, ASO titers were negative, and ANA was negative. She required a second PRBC transfusion but her hemoglobin subsequently improved without specific treatment. By discharge, Hb improved to 8.4 and platelet count to 215, BUN/Cr to 9/0.5, and fevers had resolved. Outpatient follow-up visits to hematology-oncology clinic showed continued resolution of fevers and improvement in anemia. ADAMTS13 activity was later found to be >100.0.
Discussion: Cold agglutinin disease (CAD) is a type of autoimmune hemolytic anemia (AIHA) caused by IgM autoantibodies that react with red blood cell (RBC) antigens. This occurs most readily at a temperature of 3-4C. It can manifest as hemolytic anemia, venous thromboembolism, or cold-induced symptoms, such as acrocyanosis and Raynaud phenomenon. Infections have been associated with CAD, including Mycoplasma pneumonia, Epstein-Barr virus, and cytomegalovirus. More recently, COVID-19 has been associated with CAD in adults. Patients afflicted with COVID-19 associated CAD have manifested thrombotic events, hemolytic anemia, and cerebrovascular disease. In addition to supportive care and PRBC transfusions, patients have been treated with treatments specific to COVID-19, corticosteroids, rituximab, and plasma exchange. However, this is the first case of COVID-19 associated cold agglutinin disease described in the pediatric population.
Conclusions: Cold agglutinin disease should be considered as the cause of autoimmune hemolytic anemia occurring in the setting of acute pediatric COVID-19 infection.