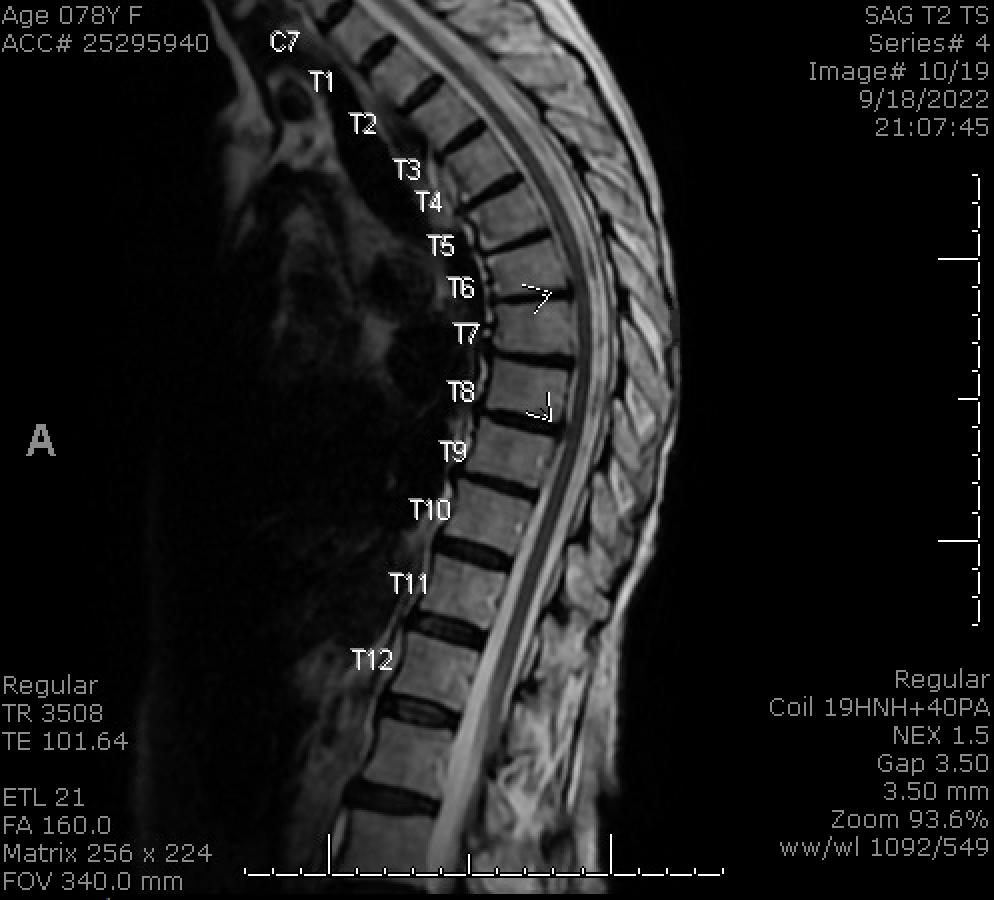
Case Presentation: A 78-year-old woman with medical history of atrial fibrillation, hypertension, hyperlipidemia, and osteoporosis presented with left lower extremity weakness and left thigh numbness. The patient was walking when she felt lightheaded and developed left thigh tingling followed by left leg weakness. She presented the next day unable to walk independently. On physical exam of the left lower extremity, strength was 4/5 for flexion and extension of the hip and knee, sensation to light touch was diffusely decreased, and Babinski sign was positive. Laboratory workup including ESR, CRP, CK, vitamin B12, and ANA were within normal limits. Brain MRI was unremarkable. Initial spinal MRI showed a non-specific, non-enhancing lesion with T2 hyperintensity at T5-6. Further serum and CSF evaluation including anti-MOG and anti-AQP4 antibodies, ACE level, and oligoclonal bands was negative. Due to progression of symptoms including urine retention, MRI was repeated on hospital day 10 which demonstrated left parasagittal and posterior cord signal abnormality at T5-T6 with T2-hyperintensity and pathologic contrast enhancement. She denied any recent infectious event or common infectious symptoms. However, she had received COVID and influenza vaccines 6 days prior to symptom onset. She was diagnosed with transverse myelitis (TM) and started on intravenous methylprednisolone 1 gram daily for 5 days with improvement in weakness and sensation.
Discussion: TM is a rare inflammatory demyelinating disease associated with systemic autoimmune disorders, infection, and vaccination.(1,2) Diagnosis is based on characteristic T2 hyperintense lesions on MRI, neurologic symptoms attributable to the lesion, evidence of inflammation such as pathologic contrast enhancement, and exclusion of spinal cord compression.(3) TM has been documented following COVID vaccines and can present after first or subsequent doses.(4-6) It is proposed that CNS demyelinating syndromes after vaccines may involve molecular mimicry or autoimmune reactions between SARS-CoV-2 spike protein antibody and human tissue.(7-8)We present a case of TM after COVID and flu vaccination. The patient had previously received the Moderna (12/2020, 01/ 2021) and Pfizer-BioNTech (10/2021, 04/2022) COVID vaccines. She developed symptoms 6 days after receiving the bivalent Pfizer-BioNTech booster and a seasonal influenza vaccine in September 2022. Of note, initial MRI of her spinal cord lesion was non-enhancing and non-specific. Given progression of symptoms and lack of an alternative diagnosis, repeat imaging was obtained which demonstrated an enhancing lesion consistent with TM. Parainfectious and post-vaccination myelitis often have nonspecific findings on MRI. While TM typically presents with long-segment T2 hyperintensity with enhancement, enhancement is more common in subacute stages than at initial presentation.(9) Within the framework of high value care, repeat imaging should be considered when there is a high index of suspicion for TM.
Conclusions: Acute TM is a rare but devastating complication of COVID infection and vaccination. Patients presenting with characteristic findings should be asked about triggers including infection and vaccination, including the increasingly common combination of COVID and flu vaccination. In addition, post-vaccination TM may present with nonspecific MRI findings, and clinicians with a high index of suspicion should consider the value of reimaging for diagnosis and treatment.