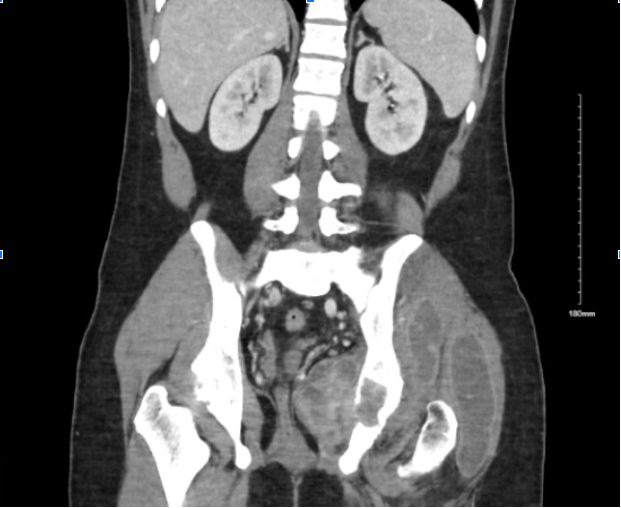
Case Presentation: A 22-year-old Filipino man presented with worsening left groin and hip pain 2 weeks after falling down 3 steps on subway stairs. Since the fall, he had minimal range of motion due to pain and required assistance with ambulation. He also reported intermittent dull achiness in that hip one week prior to the fall. On exam, he was afebrile and had severely reduced range of motion in the left hip. There was no swelling or erythema over the hip. Labs were significant for white cell count of 15,000/mcL, ESR of 64 mm/hr, and CRP of 102 mg/L. CT scan of the hip showed a 4.5 cm lytic lesion of the posterior acetabulum along with osteopenia and multiple soft tissue masses in the region surrounding the left hip. Upon further questioning, the patient reported having night sweats and subjective fevers for the past month. The presence of a lytic lesion in an otherwise young healthy man raised concern for a malignant or infectious etiology. The joint space was aspirated, draining purulent fluid which initially showed significant lymphocyte predominance and increased LDH, but AFB cultures were negative and no organisms were seen. Quantiferon test was positive, but the patient did not have pulmonary symptoms and had a clear chest X-ray. The patient was started on empiric antibiotics targeted at a pyogenic process while work-up was ongoing for other potential etiologies. Further fluid analysis revealed significantly elevated Adenosine Deaminase. Subsequently, Mycobacterium Tuberculosis PCR of the fluid confirmed tuberculosis of the joint. The patient was started on rifampin, isoniazid, pyrazinamide, and ethambutol for acetabular tuberculosis and discharged with outpatient ID follow-up.
Discussion: Pulmonary Tuberculosis (TB) is the most common location of TB, but the incidence of extra-pulmonary TB is increasing worldwide and currently makes up about 20% of all cases (1). Moreover, musculoskeletal tuberculosis comprises only a small proportion of extra-pulmonary tuberculosis (2) and usually only involves the vertebral column and only rarely involves the appendicular skeleton. Pathogenesis of this disease can be from hematogenous spread of a primary pulmonary infection, but can also be due to lymphatic drainage or due to a contiguous focus of disease. The presentation is often vague and insidious in nature, with pain often the only presenting symptom. Typical non-specific tuberculosis symptoms such as fever, night sweats, and weight loss are often absent until the late stages of musculoskeletal tuberculosis. Imaging initially may only appear as non-specific osteolysis which may mimic malignancy. In our case, an incidental fall revealed a pathologic fracture in a previously healthy young man. Patient’s recent immigration from an endemic area and a positive quantiferon test raised suspicion for TB. Empiric antibiotics were stopped as the clinical picture was not consistent with a pyogenic process and further fluid analyses confirmed our suspicion of tuberculoid fracture.
Conclusions: Though increasing in prevalence, extra-pulmonary tuberculosis remains challenging to diagnose and requires a high index of suspicion. Failure to diagnose and treat tuberculosis of the bone can lead to further bone destruction and neurologic defects.