Creating a Best Practice for Discharges Against Medical Advice
Background: Nationally, 1-2% of medical discharges from hospitals are against medical advice (AMA). Patients that leave AMA are at higher risk for readmission and adverse health events. At our facility, FY 2014 data revealed that 1% of discharges from the medical/surgical wards were AMA. The 30 day readmission rate was 44% and there was an 11% mortality rate at the time of data collection.
Purpose: Lacking a standardized approach to the discharge of patients leaving AMA, our goal was to create a best practice process for all AMA discharges. We created a patient-centered model that embraces shared decision making with emphasis on decisional capacity assessment, informed consent discussion, and patient safety at discharge.
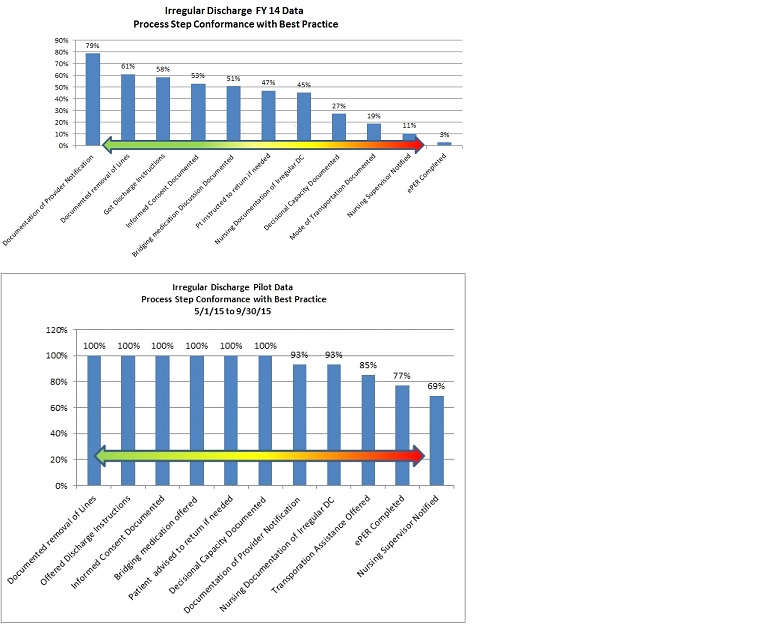
Description: A multidisciplinary team was formed to analyze the current state of our irregular discharge process (AMA and Elopement) and was charged to develop the “ideal” future state. We identified 11 key elements as goals for each AMA discharge. Future state process maps were created and 2014 data was analyzed to determine our baseline performance on the key elements (FY14 Data). Data presented is only for AMA discharges, as elopement was a rare event.
Multiple inconsistent policies related to AMA discharges were simplified into one comprehensive policy. Complimentary electronic note templates were developed for both providers and nursing to ensure that performance and documentation of the key elements were completed at discharge. The physician note emphasizes assessment and documentation of decisional capacity and the informed consent discussion. The nursing note focuses on performance and documentation of patient safety measures such as line removal, assistance with transportation and review of discharge instructions. We discontinued the use of the AMA forms as these can often create adversarial relationships. Educational sessions were held with providers, trainees and nursing staff.
Conclusions: A pilot study was completed from May to September 2015, in which our process was utilized 13 times. Data for these 13 patients is shown (Pilot Data). There was significant improvement in all key elements identified as best practice. The 30 day readmission rate was 17%; mortality data pending . The quality of documentation for informed consent and decisional capacity was markedly improved. Based on the favorable pilot data, the process is being adopted throughout the facility. Key elements scoring less than 80% will be future focus areas.