Background: Electronic medical record (EMR) chart notes are primary tool through which providers communicate their thought processes, clinical decision making and care plans. Our health system consists of 11 hospitals ranging from large academic medical center to small hospitals in Minnesota and Western Wisconsin. Hospital Medicine team represent over 250 providers across all the sites. Over years different hospitalist providers have tailored their note templates leading to significant variation even at same site and challenges during care transitions. Variation in notes also leads to difficulties for other care team members (consultants, nurses, care management) to find information in hospital notes.
Purpose: Our aim was to create and implement standardized note templates for all notes (H and P, progress, consult, discharge) notes for all hospitalist across system. The initiative was driven by multiple goals including enhancing provider efficiency, improving ease of use across different sites, making care transitions (H and P to progress note) more efficient, automatic capture of key diagnosis impacting case mixed index and ultimately improve patient care. We also made this part of our annual care initiative program for hospitalists with bonus if meet goals.
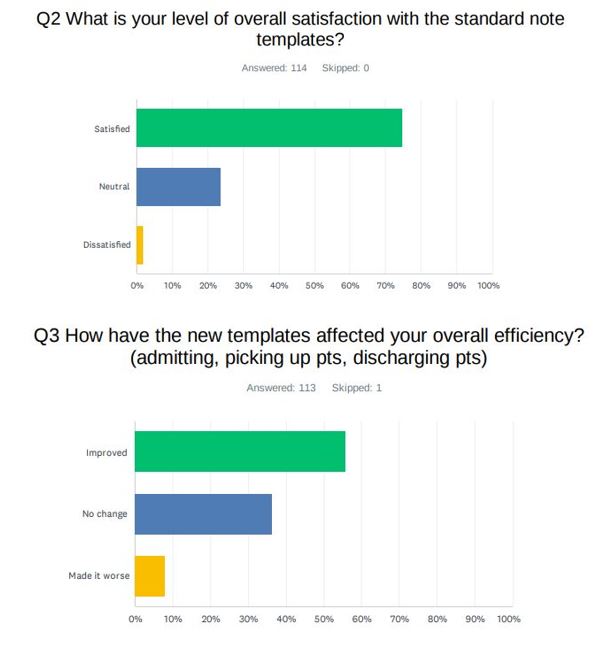
Description: We formed a permeant committee in December 2023 representing hospitalists from each site, informatics MD and safety-quality medical directors. We named this committee (H-ON, Hospitalists Orderset and Notes committee) with primary goal of creating new note templates and maintaining them long term. Committee met every other week and created standard note templates for use across the system in Q1 of 2024. The standard template featured uniform layout, cutting edge functionality and a novel embedded tool for compliance tracking. in early Q2 2024 note templates were trialed by selected user groups and gradually rolled out to all sites. CME events discussing features of note template was conducted. On July 1st measurement of compliance started, and goal was set at 90% note template compliance. On October 1st survey was also sent out to all hospitalists on their opinion of standard notes. After implementation note template compliance remain over 99%. Survey completed by 114 hospitalist providers showed 74.5 % hospitalists were more satisfied with new standard note templates, 23.7.% neutral and 1.7% were dissatisfied compared to previous state. On efficiency 55.7 % providers felt improved efficiency in care transitions, 36.3% neutral and 7.9% felt reduced efficiency compared to previous state.
Conclusions: With this project we were able to implement standardized systemwide hospitalist note templates in less than 6 months. Our experience and survey show standardized notes can improve hospitalists workflow and care transitions with high user satisfaction rate and self-reported improvement in efficiency by over half of the hospitalists. We are also seeing improvement in our coding performance due to standardized capture tool of electrolyte abnormalities and malnutrition diagnosis in our standard notes, similar results are seen in previous studies. (1)