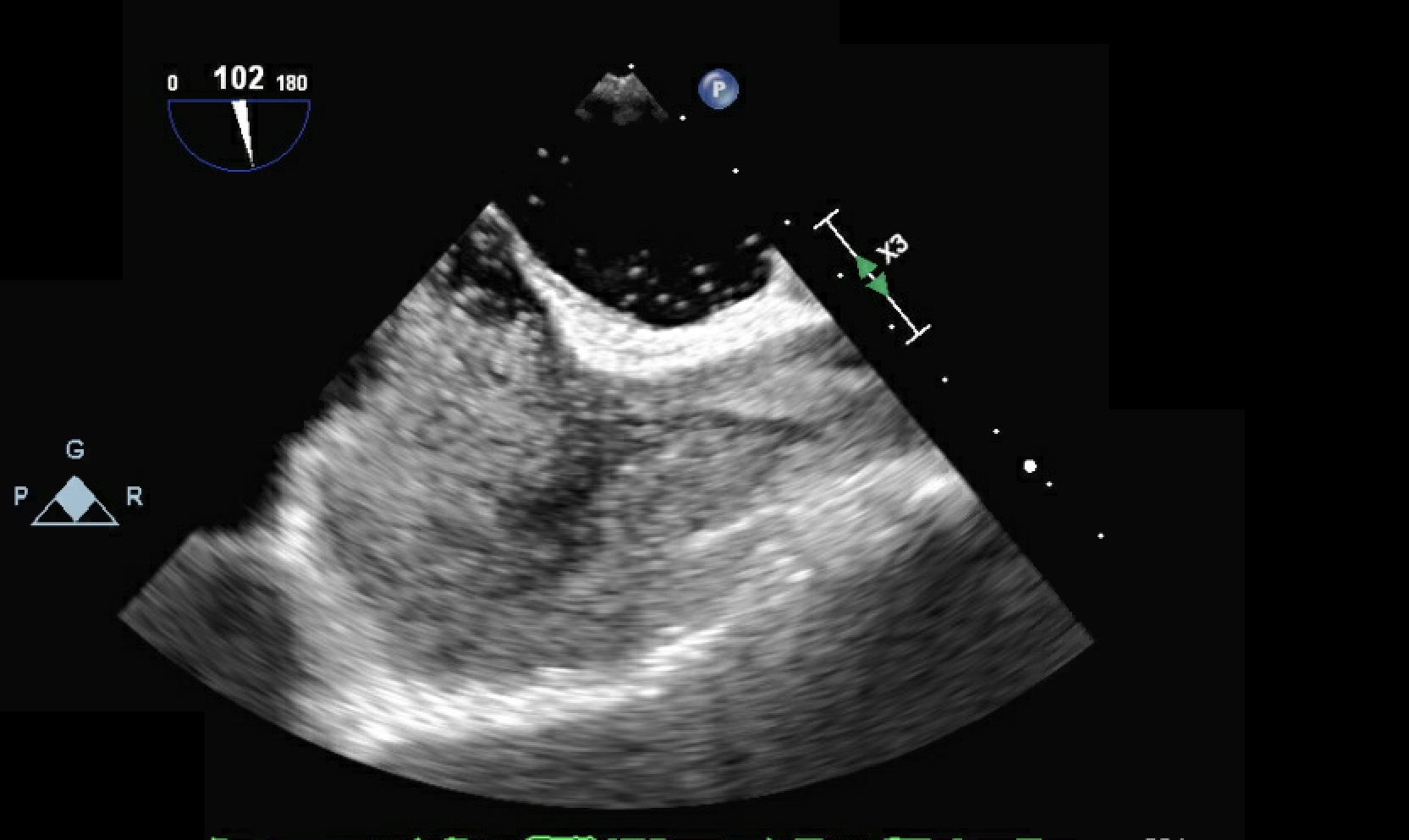
Case Presentation: Case 129-year-old male previously healthy without significant medical history had transient right-sided weakness and blurry vision for one day. Head CT scan was normal. CT angiogram (CTA) of head and neck did not reveal arterial lesion. MRI of brain revealed small acute ischemic changes in the left posterior frontal lobe. No Hypercoagulable state was identified. Echocardiogram revealed atrial septal shunt. Transesophageal echocardiography (TEE) confirmed the presence of patent foramen ovale (PFO). Lower-extremity venous duplex ultrasound (VDUS) was negative. He was discharged with dual antiplatelet therapy (DAPT) with aspirin and clopidogrel, atorvastatin and the appointment for PFO closure. Case 259-year-old man without cardiovascular disease presented for intractable occipital headache and gait instability. CT of the head revealed right posterior inferior cerebellar artery (PICA) territory infarction. CTA of head and neck showed vertebral arteries were right dominant and distal left vertebral artery was atretic. Echocardiogram revealed an atrial left-to-right shunt. TEE identified the PFO with an interatrial septal aneurysm and a bidirectional shunt. Lower-extremity VDUS did not identify any thrombus. The patient was started with aspirin, atorvastatin and a 30-day cardiac monitor to screen for paroxysmal atrial fibrillation before proceeding with PFO closure.Case 375-year-old man with a past medical history of hypertension presented with acute expressive aphasia. The word-finding difficulty lasted for an hour. CT of the head was normal. Bilateral carotid duplex scan was unremarkable. Echocardiogram showed PFO with right-to-left shunting and aortic sclerosis and calcification. TEE showed an intra-atrial septal aneurysm with PFO and bidirectional shunt. The patient was discharged with aspirin, atorvastatin and a 30-day loop monitor.
Discussion: We demonstrate different approach to patients of various age groups that were found with cryptogenic stroke associated PFO. Several studies have shown a higher prevalence of PFO in cryptogenic stroke patients. Increasing evidence suggests that PFO closure can reduce future stoke risk in selected patients. There is no clear evidence in managing PFO in cryptogenic stroke patients. The consensus now is to provide PFO closure for cryptogenic stroke patients under age 60. In our case series, the younger patient was advised to opt for PFO closure and the older patients had a more conservative management. Clinician should review the risk and benefit of different treatments with the patients to facilitate shared decision making.
Conclusions: Patients with cryptogenic stroke should be evaluated for PFO. Personalized management and shared decision making are recommended for PFO management in these patients.