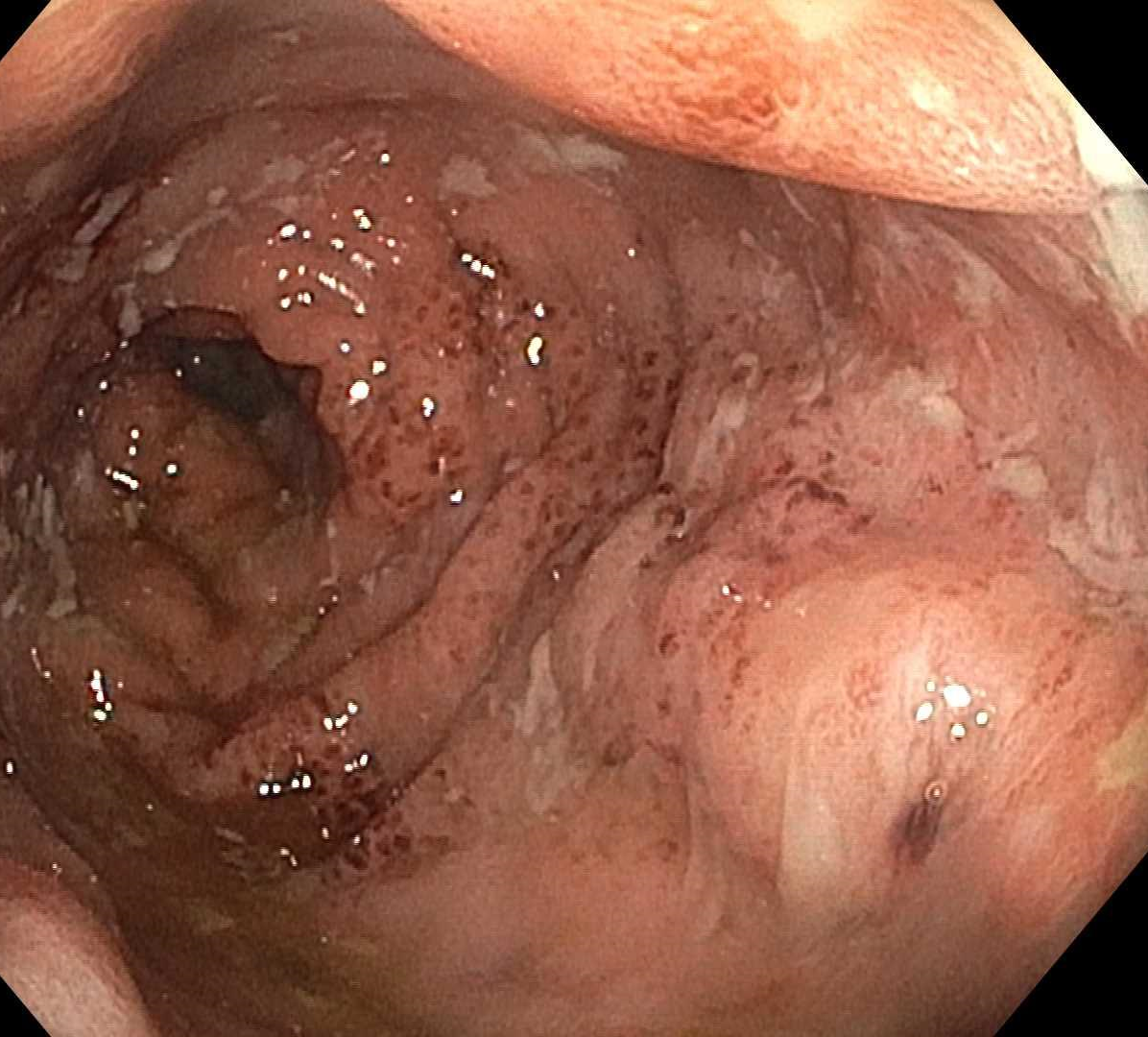
Case Presentation: A 62-year-old male patient with a history of heart transplant nine years ago on mycophenolate mofetil (MMF) presented for chronic diarrhea with increasing frequency, urgency, incontinence, sporadic melena, and fevers. He tested positive for Clostridium difficile (C. diff) toxin and improved on fidaxomicin. Soon after discharge, he required rehospitalization for worsening symptoms. A colonoscopy found multiple well-defined punched out ulcers throughout the colon. CMV and HSV tests staining were negative. Biopsies demonstrated active chronic colitis with ulceration. Based on a Naranjo score of 7, his diagnosis was suspicious for MMF-induced colitis. He was switched from MMF to mycophenolic acid, with improvement in symptoms. However, the patient continued to have multiple rehospitalizations for worsening symptoms which mildly improved with an empiric trial of budesonide. Despite this, he had a Harvey Bradshaw score of 16 during a follow-up GI clinic visit. A repeat colonoscopy was performed that showed persistent colitis with normal terminal ileum, and the biopsies showed chronic colitis with noncaseating granulomas. His symptoms resolved on infliximab and subsequent Harvey Bradshaw score was 1 during a GI clinic follow-up.
Discussion: Solid organ transplant recipients (SOTr) often have diarrhea as a result of dehydration, medication side effects, or infection secondary to immunocompromised state. De novo inflammatory bowel disease (IBD) is rarely seen as a cause of diarrhea in transplant patients but has been documented in SOTr. Timely identification of diarrheal cause in this patient population is necessary to avoid significant morbidity including possible organ rejection.Diarrhea carries a prevalence of 20-50% among SOTr and increases their risk of morbidity and mortality. The most common causes include medications used in transplant medicine and infection from the resulting immunocompromised state. MMF, a common immunosuppressant drug used in transplant patients, causes diarrhea in up to 36.1% of patients. MMF-colitis is known to mimic IBD, graft-versus-host disease, ischemic colitis, or infectious colitis. Common infectious agents include C. diff, Cryptosporidium, CMV, HSV and norovirus. This patient’s heart transplant history, persistent evidence of C. diff infection, and use of MMF complicated accurate diagnosis and treatment of his symptoms. Notably, few cases of Crohn’s have been reported among heart transplant patients, making the final diagnosis challenging. The patient was ultimately found to have biopsy-proven Crohn’s disease on repeat colonoscopy and resolution of symptoms with infliximab.
Conclusions: Multiple confounders can exist in the diagnostic workup of colitis in transplant patients. This case emphasizes the need to have a lower threshold of clinical suspicion for inflammatory bowel disease as part of the differential diagnoses in heart transplant cases, despite its rarity.