Background: Community acquired pneumonia (CAP) is one of the most common causes of hospitalization in the United States1 and a frequent source of antibiotic overuse.2 Two thirds of patients hospitalized for CAP receive excess antibiotic duration, primarily from excess therapy at discharge.3 Patients living in rural areas are known to have worse health outcomes than those in urban settings,4 including inappropriate antibiotic prescriptions.5 While there are multiple potential drivers of antibiotic overuse in patients living in rural areas—one may be clinician concern about lack of access to follow-up care, leading to “just in case” prescriptions. Our objective was to determine whether clinicians disproportionately prescribe excess antibiotic duration at hospital discharge to patients living in rural areas as compared to patients in local urban settings.
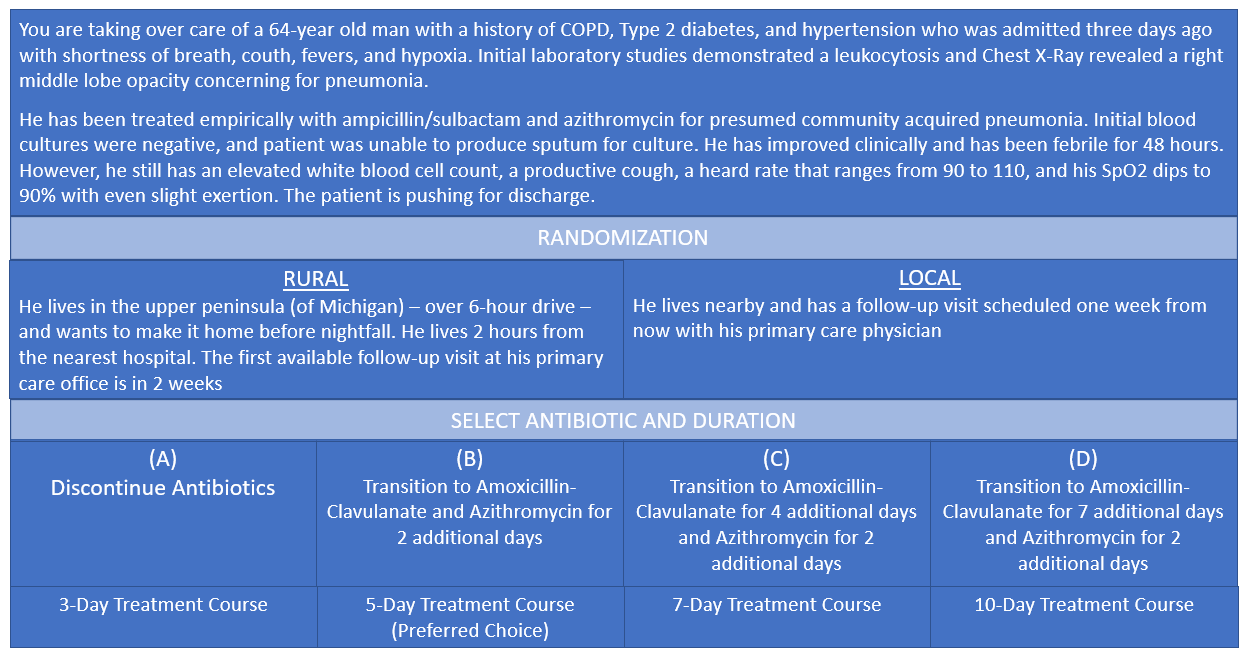
Methods: As part of a larger study on antibiotic stewardship and care transitions,6 hospitalists working at a single large academic medical center were surveyed in November 2019 using Qualtrics XM. Participants were asked to respond to a clinical vignette regarding their preferred discharge antibiotic duration for a 64-year-old patient hospitalized for pneumonia who, though improved, remained ill but is requesting discharge (Figure 1). Respondents were randomized to receive one of two additional pieces of information: a) Rural scenario, the patient lived at least six hours away, two hours from the nearest hospital, and was unable to see his primary care doctor for two weeks or b) Local scenario, the patient lived nearby with primary care follow-up available in one week. According to guidelines,7 this patient should receive a five-day treatment course. Therefore, we defined 5-days as appropriate and 7-10 days as excess duration. We compared appropriate vs excess duration with a chi square test.
Results: Among 102 hospitalists surveyed, the response rate was 70% (71/102). Survey respondents were 42% female (30/71), practiced hospital medicine for a mean of 6.9 years, and spent on average 90.5% of their effort on an inpatient medicine service. Twenty-nine hospitalists (41%) received the rural scenario and 42 (59%) received the local scenario. Responses are shown in Table 1. In all, participants randomized to the rural scenario were more likely to choose an excessive (7-10 day) antibiotic duration than were those randomized to the local scenario (37% [11/29] vs. 10% [4/42], respectively, P=0.004).
Conclusions: In this randomized vignette, hospitalists were more likely to prescribe guideline-discordant, excess antibiotic duration for patients residing in rural settings with poor follow-up compared to patients in local urban settings. Our findings demonstrate that clinicians take into account a patient’s life context when making decisions about antibiotics.8 They also suggest a cognitive bias that longer duration is protective, despite evidence that it increases risk of harm (including Clostridioides difficile infection) post-discharge.2,3,9 Our study was conducted prior to the COVID-19 pandemic, when use of telemedicine (which could improve access) increased.10–12 Antibiotic stewardship is more challenging in rural settings for myriad reasons.5 These results suggest that clinician concern regarding access to care may contribute to antibiotic overuse for patients residing in rural areas. Stewardship should better integrate the social determinants of health into intervention design to ensure all patients receive optimal antibiotic therapy.