Background: Catheter occlusion is one of the most common complications associated with Peripherally Inserted Central Catheter (PICC) insertion, affecting 1 in every 8 PICCs placed. Occlusion may have important consequences for patients including inability to use the device, delays in tests or treatment, or if irreversible the need to remove and replace the device. Based on data from the Michigan Hospital Medicine and State Consortium (HMS), a large state-wide quality improvement collaborative, 12% of the 14,000 PICCs experienced a catheter occlusion during the life of the catheter. One in five (21%) of these occluded devices had to be removed due to irreversible occlusion. Additionally, $250,000 was incurred in tissue plasminogen activator (tPA) costs to de-clot catheters. These findings suggest that efforts to prevent catheter occlusion can not only help reduce costs but might also substantially improve patient safety.
Purpose: To describe the impact of multi-model quality improvement initiative on decreasing PICC-related catheter occlusion in a large urban community teaching hospital.
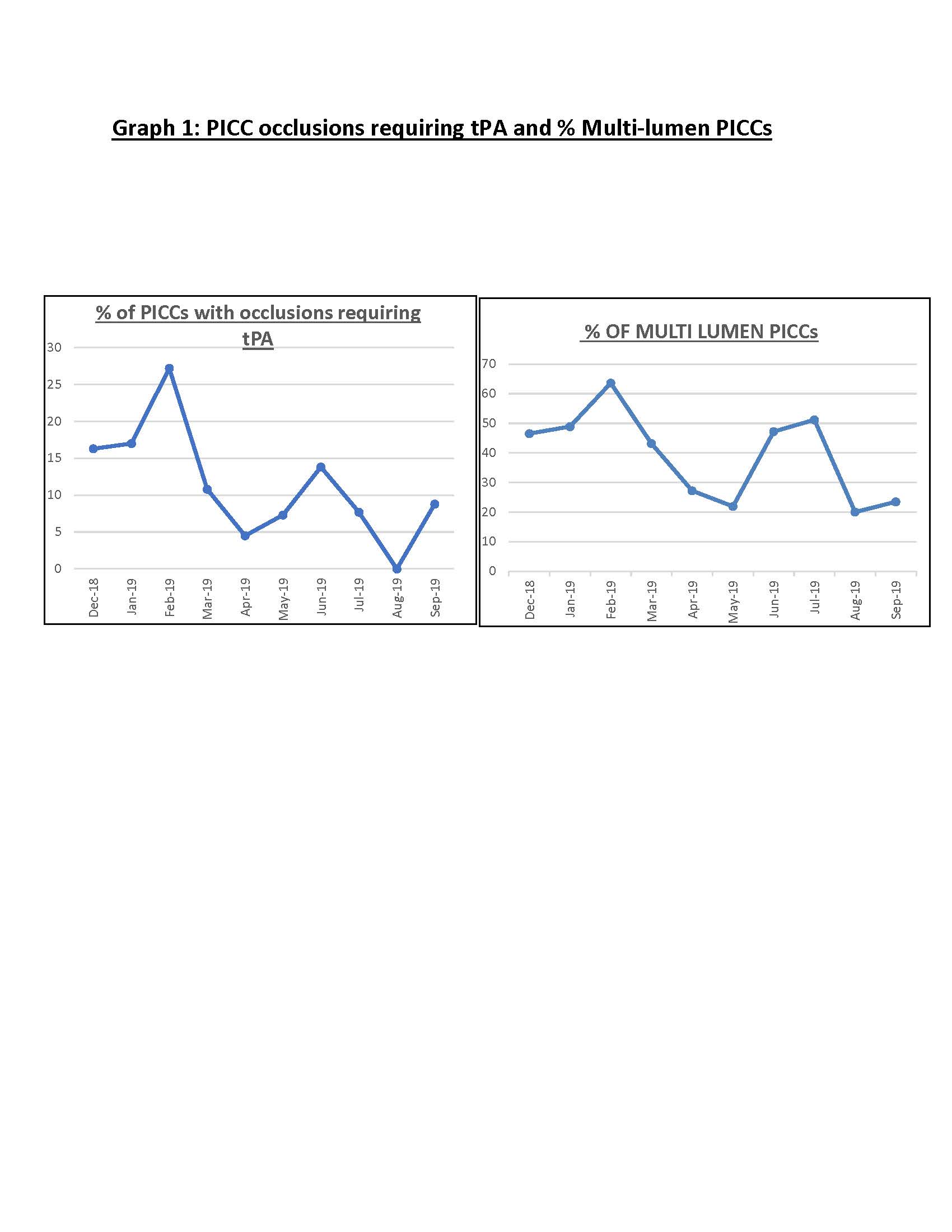
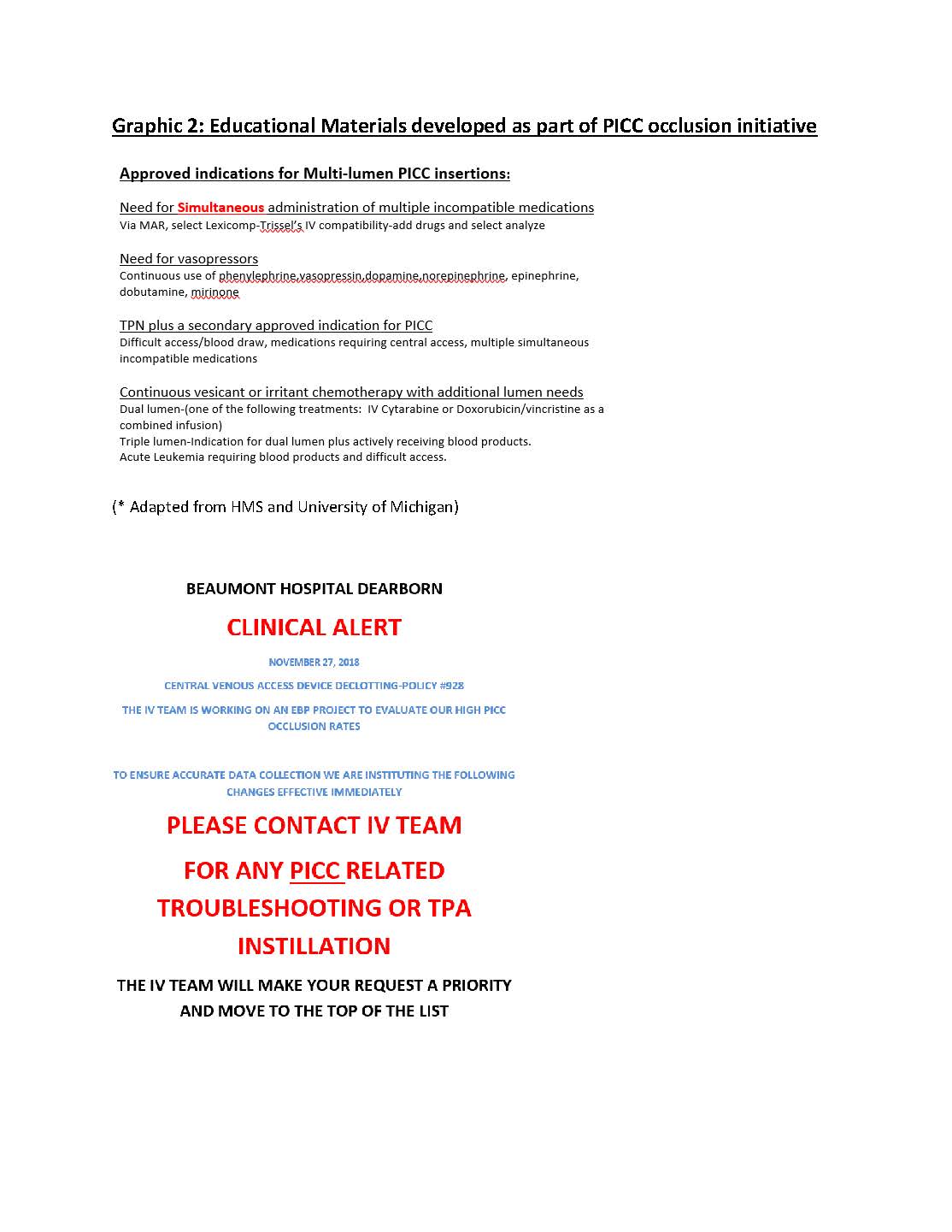
Description: In 2018, our institution placed 470 PICCs with 71 incidents of tPA use resulting in an occlusion rate of 15.1%, significantly higher than the HMS collaborative average of 12%. Review of occlusions found multi-lumen catheters, inadequate flushing and troubleshooting techniques as key contributing factors akin to modifiable factors identified in other catheter occlusion studies. Starting January 2019, our vascular access team implemented a hospital-wide multi-modal intervention that included the following components: decreasing number of PICC lumens, educating nurses on using the SASH (Saline, Administer medication, Saline, Heparin) flushing technique; and directing all tPA use to the vascular access team. Educational strategies included clinical alerts and catheter maintenance tips as part of daily huddles and nursing mandatories. The vascular access team also re-organized their staffing to prioritize troubleshooting vascular access catheters and prevent delays in care. Finally, the vascular access manager provided individualized feedback to nursing unit managers on cases where tPA was used prematurely without appropriate indication or prior troubleshooting by the vascular access team. Consequent to these efforts, year to date in 2019, we have seen a 33% decrease in our occlusion rate with 38 incidents of TPA use in 375 PICCs (10.1% compared to our baseline of 15%). Graph 1. Concomitantly, a decrease in multi-lumen catheter use especially in non-critical care units has been observed. A spike in catheter occlusions seen in June 2019 was primarily driven by multi-lumen catheter and premature tpA use in critical care environments. Efforts to engage clinicians in these areas and electronic medical record modifications to hardwire efforts are ongoing.
Conclusions: A multi-modal vascular access driven initiative focused on education, decreasing number of lumens and appropriate flushing can decrease catheter occlusion rates and improve safety of vascular access in hospitalized patients.