Background:
Effective communication among providers and patients during the hospital discharge process is critical to patient care. Anticoagulation has proven to be an effective therapy for several medical conditions, but communication deficits regarding anticoagulation may lead to adverse patient outcomes following hospital discharge. The aim of this study was to evaluate the quality of information transfer regarding anticoagulation therapy and monitoring across an integrated health care delivery system.
Methods:
Evaluation of randomly sampled discharge documentation packets of patients discharged from all 5 acute care hospitals of the Partners Healthcare System to subacute facilities. Reviewers were a mix of trained medical residents at acute sites and admitting physicians at receiving subacute sites. Results were calculated as proportions and 95% confidence intervals.
Results:
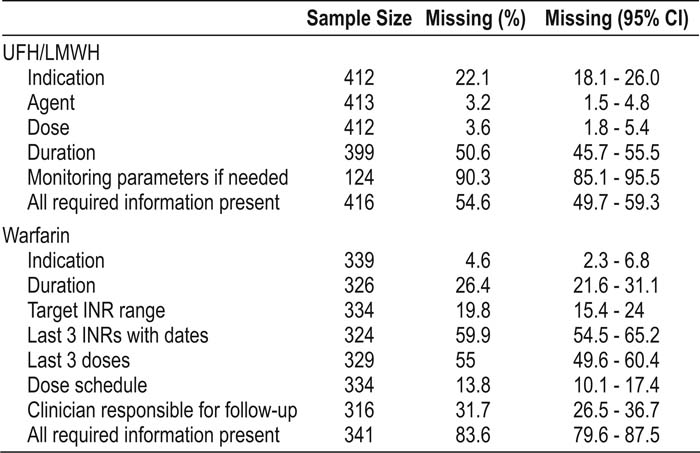
Of 757 patients prescribed anticoagulation at discharge from March 2005 through June 2007, 341 were prescribed warfarin, and 416 were prescribed unfractionated heparin (UFH) or low‐molecular‐weight heparin (LMWH). Deficits were found in each of the data elements required to safely prescribe anticoagulation (Table 1). Of the patients prescribed UFH/LMWH or warfarin, 45.4% and 16.4%, respectively, had all the required information in the discharge summary. Patients discharged from surgical services were more likely to have complete information regarding the use of warfarin than were patients discharged from medical services (odds ratio [OR] 2.35, 95% confidence interval [CI] 1.29‐4.29). The 3 Partners community hospitals were more likely to discharge patients with all the required information for warfarin than were the 2 academic medical centers (OR 1.85, 95% CI 1.36‐2.53).
Conclusions:
Important information to safely prescribe anti‐coagulation after discharge was often missing from the discharge summaries of patients transferred from acute hospitals to subacute facilities. Information regarding the use of warfarin was more likely to be incomplete than that for UFH/LMWH. For warfarin, information was more likely to be incomplete on medical services compared with surgical services and from academic medical centers compared with community sites. For patients prescribed anticoagulation therapy at hospital discharge, greater efforts are needed to communicate the clinically relevant information to those providing continuing care.
Author Disclosure:
G. Esteban, none; T. Moniz, none; J. Ungar, none; J. Lee, none; M. Chan‐Macrae, none; J. Schnipper, none.