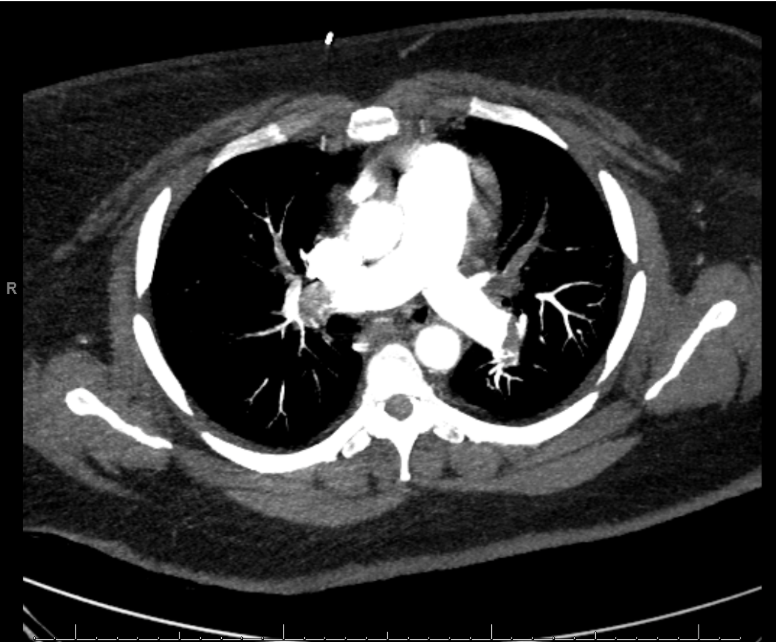
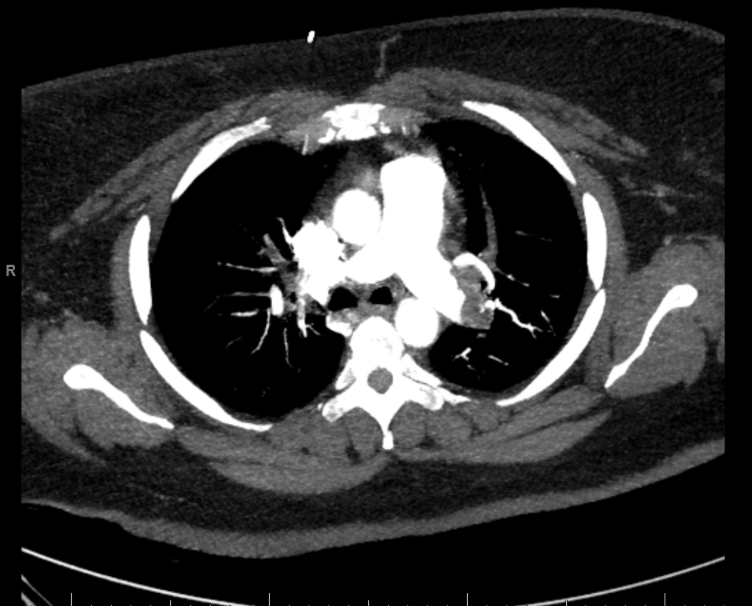
Case Presentation: Cardiopulmonary resuscitation (CPR) is a critical intervention in cardiac arrest management, essential for maintaining circulation and oxygenation to avert irreversible brain damage. This case report highlights the impact of high-quality CPR on neurological outcomes, even after extended resuscitation.A 45-year-old sedentary female with multiple sclerosis (MS) and morbid obesity with a BMI of 53 presented with gastrointestinal and dyspnea symptoms post-immunotherapy. Imaging identified bilateral lower lobe pulmonary embolisms and a saddle embolus with significant thrombus burden and right heart strain. During suction thrombectomy, the patient experienced pulseless electrical activity (PEA) arrest. Manual CPR was immediately initiated, and the patient was intubated 12 minutes later. Due to the patient’s body habitus, robotic compressions could not be performed. Sustained return of spontaneous circulation (ROSC) was achieved after 70 minutes, despite transient ROSC episodes. Throughout the resuscitation, she received 13 doses of epinephrine and 4 doses of sodium bicarbonate. Following the event, the patient required hemodialysis due to renal deterioration but stabilized hemodynamically five days later. She regained cognitive capacity and full motor function within 10 days, leading to discharge after a 28-day hospitalization.
Discussion: The optimal duration of CPR in adults remains debated. A 2024 meta-analysis indicated a significant decrease in favorable neurological outcomes beyond 15 minutes of CPR. Effective CPR entails compressions at a depth of at least 2 inches at a rate of 100 to 120 compressions per minute, full chest recoil, minimal interruptions, and proper team coordination. Despite typically poor outcomes associated with prolonged CPR, this case illustrates that timely and effective resuscitative efforts can result in complete neurological recovery even after 70 minutes of CPR. A retrospective cohort study in 2024 found the probability of favorable outcomes beyond 32 minutes of CPR to be less than one percent, highlighting the exceptional nature of this case.
Conclusions: This case report attenuates the importance of high-quality CPR in achieving positive neurological outcomes, challenging conventional beliefs about prolonged resuscitation prognoses. It reinforces the need for rigorous adherence to CPR guidelines, ongoing education, and training for medical providers. The remarkable recovery of this patient emphasizes the potential for favorable outcomes with persistent and effective resuscitative efforts. Further research is warranted to refine CPR duration guidelines and explore factors contributing to improved patient outcomes. Studies investigating predictive factors for favorable neurological outcomes and the efficacy of mechanical compression devices are planned.