Background: Risk of having a major adverse cardiac event in the perioperative period is known to be raised among those with underlying cardiovascular disease undergoing noncardiac surgery. ACC/AHA 2014 guideline is an excellent tool for the physicians to evaluate perioperative cardiac risk. However, the evidence-based set of algorithms are often under- or inappropriately utilized due its complexity, especially in specific patient populations.(e.g., history of coronary intervention.)
Purpose: Among multiple electronic tools designed to assist clinicians, mobile clinical decision support(CDS) apps can take advantage of non-EHR data(e.g., goal of treatment) and also be very user-friendly. We aimed to convert the ACC/AHA guideline into an interactive mobile app which offers evidence-based knowledge at the point of care and validate its clinical usefulness.
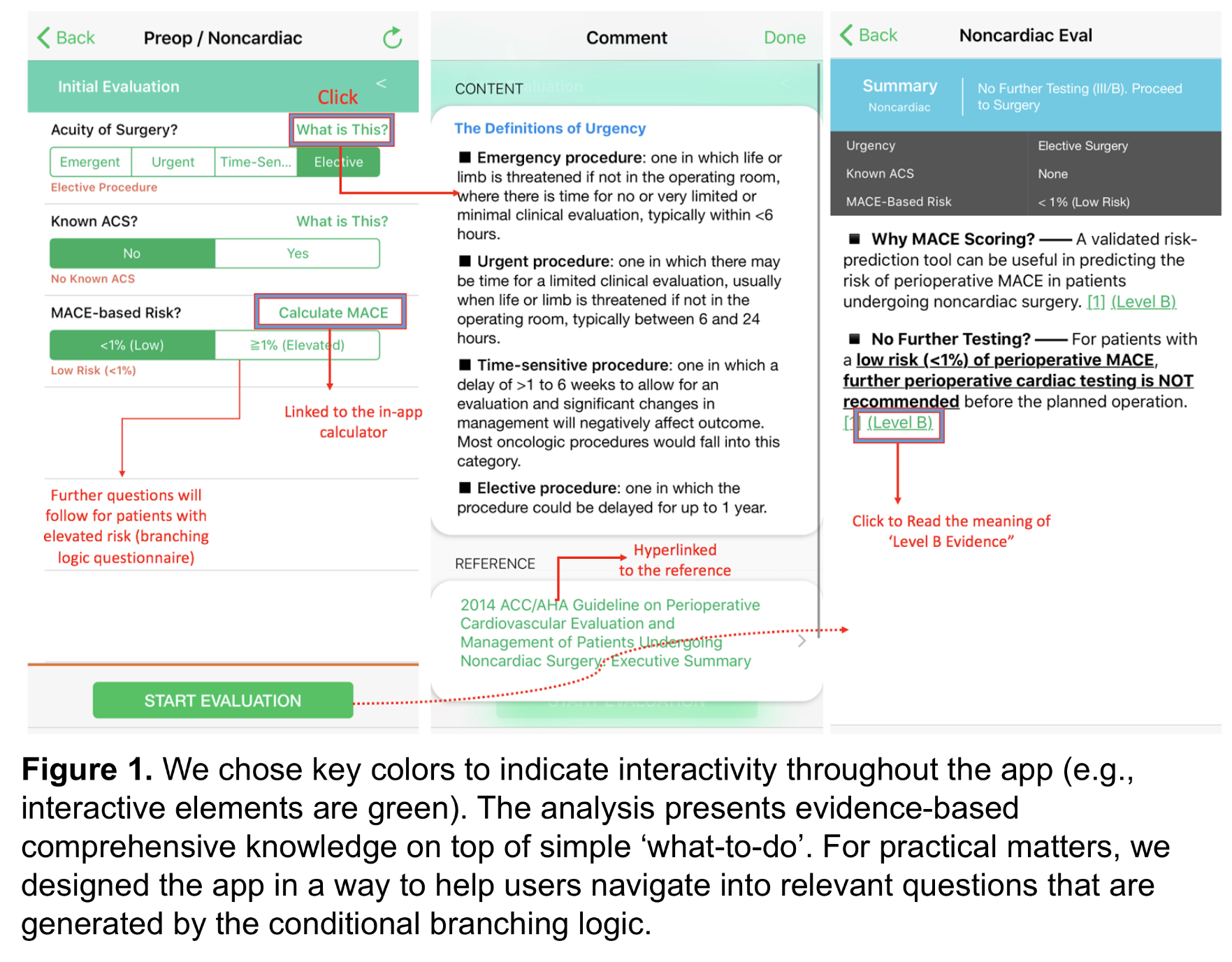
Description: We designed an app in a step-by-step process, so when the user answers one question, the app would provide the applicable next step(conditional branching logic). The first step was to build an app framework, which has the flexibility to be applicable to various problems, and also allowed easy maintenance. The design of the framework followed Human Interface Guideline(Apple Inc, 2017). For instance, we chose key colors to indicate interactivity throughout the app (e.g., interactive elements are in green, not interfering with other elements). (Figure 1) We used the Swift/XCODE environment to develop the framework. We wanted to apply the framework to build a CDS which support a simpler guideline as a testing purpose before working on ACC/AHA guideline. The prototype was a diagnostic algorithm for obstructive sleep apnea. Ten residents were recruited to assess the decision making accuracy, and 15 case scenarios were given to answer whether a sleep study was needed. The app increased the mean of decision accuracy from 68 to 93%(p < 0.0001). By using the app, each subject had 85% probability of changing its wrong decisions into the right ones (41/48), while there was only 2.9% (3/102) probability of turning the right decisions into the wrong ones. With the feedback from the users, the development team revised, and updated the design framework, user interface/experience, flexibility and maintenance issues. With that foundation, we developed this app for perioperative evaluation. We plan to conduct a randomized trial of 3 behavioral interventions, with individual clinician as the unit of randomization. Our hypothesis is that physicians with the app will make decisions more consistently on given cases compared to non-users. The secondary outcomes include: time spent on decision, rate of harmful decisions(e.g., class C harm), user satisfaction, and 1-week follow-up to investigate the persistence of educational effects. The following interventions will be compared: Mobile CDS Group(MCG) will prompt the clinicians to utilize the study application for decisions. Conventional Reference Group(CRG) is an intervention where clinicians are allows to use any web-based references(e.g.UpToDate), as well as mobile medical calculators. The last group is the control group.
Conclusions: We converted the peer-reviewed, evidence-based guideline for perioperative cardiac risk assessment tool into an interactive mobile application.