Background: Case Managers (CM) are now a standard presence in emergency departments (ED) of large hospitals, partnering with ED and Hospital Medicine providers to improve care. They are integral in improving hospital throughput and reducing unnecessary hospital admissions and readmissions. Case Managers generally identify high-risk patients using a manual chart review process or by provider request to determine whether hospital admissions are appropriate or if an alternative disposition for the patient exists. This manual case-finding process can be time-intensive and inefficient and was identified as an area of opportunity in rapid improvement events for ED CM at our institution.
Purpose: As part of our work on reducing readmissions at an academic medical center, our project aim was to develop an automated screening tool for case finding that would improve the ability of CM to identify patients at high risk for return to ED or hospitalization. This improvement in prediction could also be more efficient, allowing CM more time for interventions such as readmission reduction strategies. The Case Management Priority Score (CMPS) screening tool is a clinical innovation developed by interdisciplinary consensus opinion and we report our initial findings.
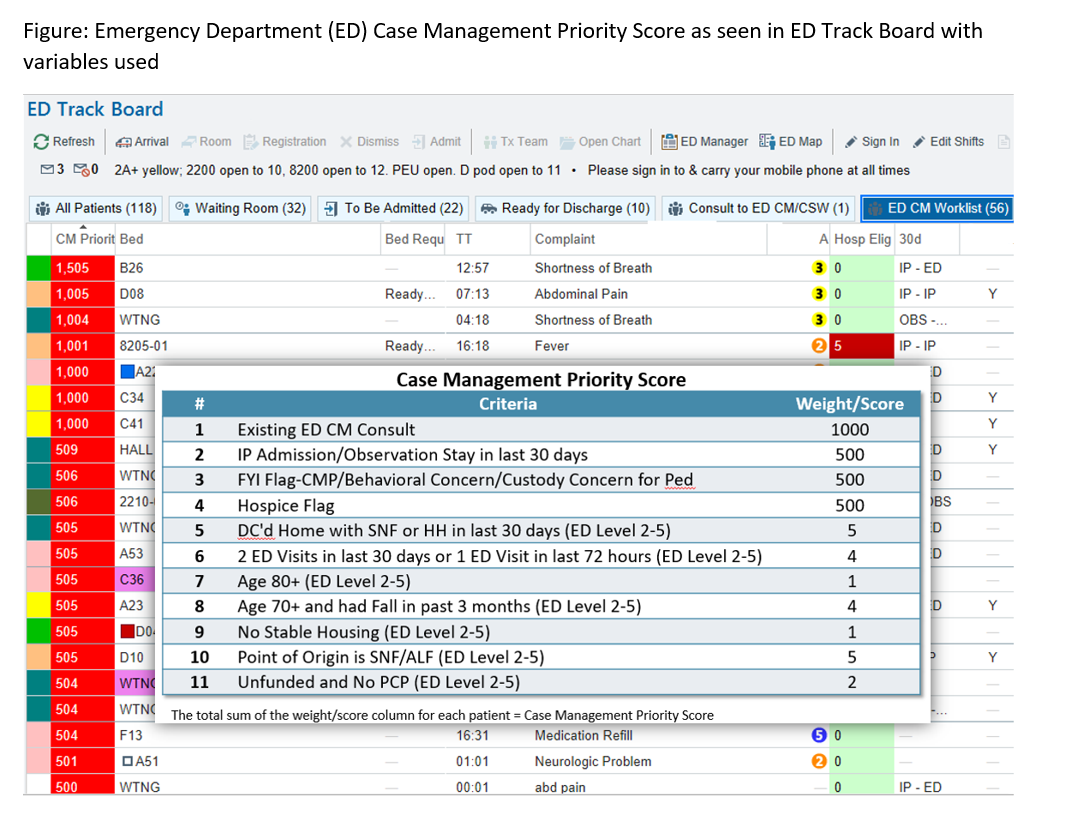
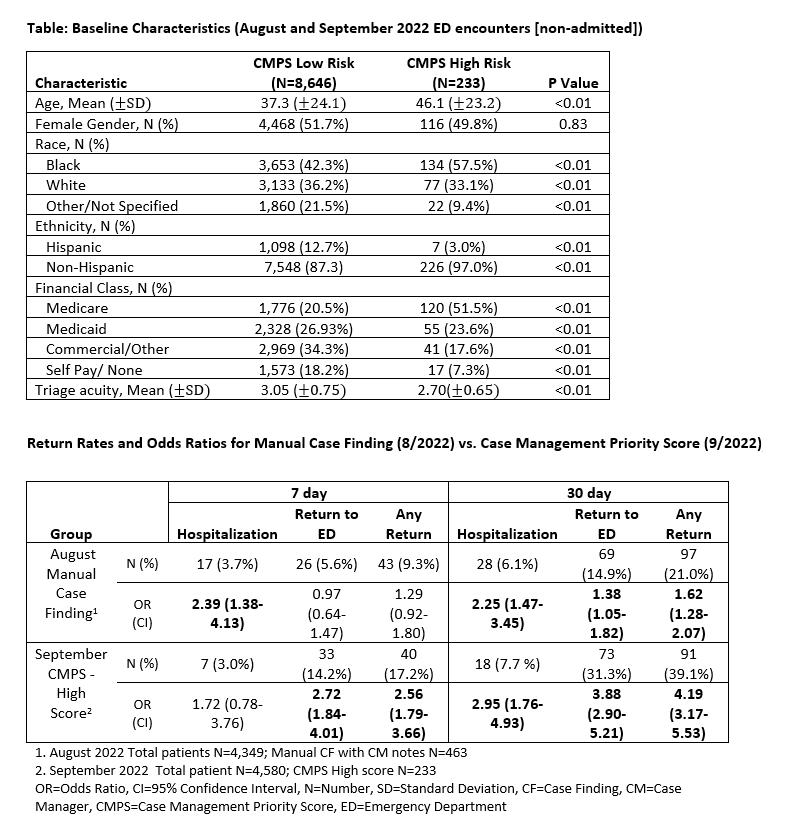
Description: Before CMPS go-live, the standard case-finding methodology used by ED CM to identify high-risk patients was manual. High risk was defined as a return to ED or hospitalization within 7- and 30- day time frames of the index ED visit. Patients thought to be high risk by ED CM using manual case-finding were indicated by documentation in the medical record. The Case Management Priority Score resides in the electronic medical record (See Image 1: Figure) and went live on 9/1/2022. Eleven demographic and utilization variables were identified and weighted to determine an overall CMPS which would guide ED CM to which patients were at high risk for returns or hospitalizations. They can hover their cursor over CMPS to discover the variables impacting the score which may help determine which interventions to apply. Four variables were weighted high enough to ensure that CM always intervened; ED consult order for CM, prior ED or hospital utilization, complex care/behavioral flags, and hospice enrolled. Image 2 (Table) shows baseline characteristics for patients scoring high risk were different than the low risk in all areas except gender. The Table also shows that, compared to the prior manual case-finding methodology (8/2022), CMPS (9/2022) had a higher odds ratio of identifying patients that were at risk for most 7- and 30- day return to ED and hospitalization outcomes. The odds ratio for any 30-day return (ED or hospitalization) for CMPS in 9/2022 was 4.19 (3.17-5.53) vs 1.62 (1.28-2.07) for manual case-finding in 8/2022.
Conclusions: In this clinical innovation project, the CMPS screening tool was found to be more predictive in identifying patients at risk for return to ED or hospitalization than manual case finding. If used by CM to identify ED patients to focus on, this may be more accurate than existing manual case-finding techniques, will help ED CM efficiencies, and help reduce returns to ED and hospitalizations. Our future focus for this work includes further analysis of the variables contributing to CMPS to refine the tool for prediction performance and develop strategies to increase its usage among CM.