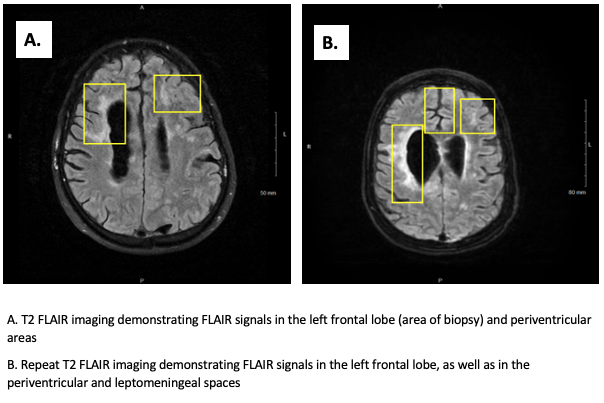
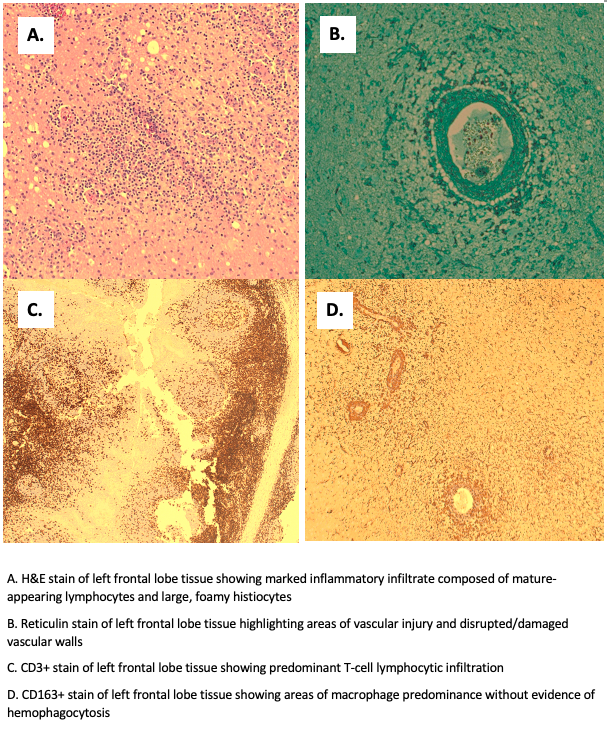
Case Presentation: A 56-year-old male with a past medical history of hemophagocytic lymphohistiocytosis (HLH), in remission following chemotherapy in 2018, left MCA CVA in 2016 without significant residual deficits, restless leg syndrome, neurodegenerative motor neuron disease with lower extremity spasticity, and peripheral neuropathy was brought to the hospital for weeks of increasing confusion and generalized weakness, and months of poor appetite with a 30 lbs. weight loss. On exam, the patient was alert and oriented to self, place, and time with intermittent confusion about the situation. There was generalized weakness without focal findings and all cranial nerves were intact bilaterally. A comprehensive lab workup, whole spine MRI, and EMG were all non-diagnostic. A continuous EEG showed moderate generalized slowing of the background without epileptiform discharges nor seizures. A brain MRI demonstrated numerous new areas of enhancement in the subcortical white matter and in the leptomeningeal and periventricular regions that were concerning for a recurrence of HLH. A lumbar puncture was unremarkable with mild lymphocytic pleocytosis (7 nucleated cells/uL) and slightly increased protein (57 mg/dL). The patient also did not meet diagnostic criteria for recurrence of HLH (negative bone marrow biopsy, below-threshold ferritin and triglyceride levels, and lack of cytopenias). Subsequently, a left frontal lobe brain biopsy of a suspected inflammatory lesion identified on the MRI was performed and confirmed primary angiitis of the CNS (PACNS) with perivascular lymphocyte and histiocyte-rich inflammatory processes and vasculitis. The patient was treated with high-dose oral prednisone and IV cyclophosphamide, and his mentation gradually improved. His treatment will be continued long-term and managed according to his clinical status by outpatient rheumatology.
Discussion: PACNS has an incidence rate of 2.4/1,000,000 person-years in North America—it is a rare heterogenous disorder of an unknown cause characterized by blood vessel inflammation in the brain and spinal cord that exists in the absence of systemic vasculitis.(1) Since it has varied clinical and pathological findings that are easily confounded by other pathologies, it is crucial to rule out numerous disorders that mimic PACNS (infections, malignancies, secondary cerebral vasculitis, vasospastic disorders, arterial and embolic diseases, leukoencephalopathies, and stroke-like syndromes). In this patient with prior HLH, its recurrence would have been a likely cause of his symptoms. By completing an extensive workup, HLH and other PACNS mimics were ruled out. The brain biopsy, though not always feasible and is difficult to perform, helped definitively diagnose PACNS and should be considered in cases of diagnostic dilemmas given the treatment implications. By correctly treating PACNS with long term high-dose glucocorticoids and cyclophosphamide (or rituximab in patients intolerant of cyclophosphamide), poor outcomes such as severe disabilities and death may be minimized.(2-4)
Conclusions: In patients with pre-existing conditions of multi-system etiologies, PACNS proves to be more complicated to diagnose and treat. This case demonstrates the importance of keeping a broad differential (including PACNS) and completing a thorough workup (including a brain biopsy) for unexplained mentation changes in patients, especially in those with a clinical history of disorders that may mimic PACNS.