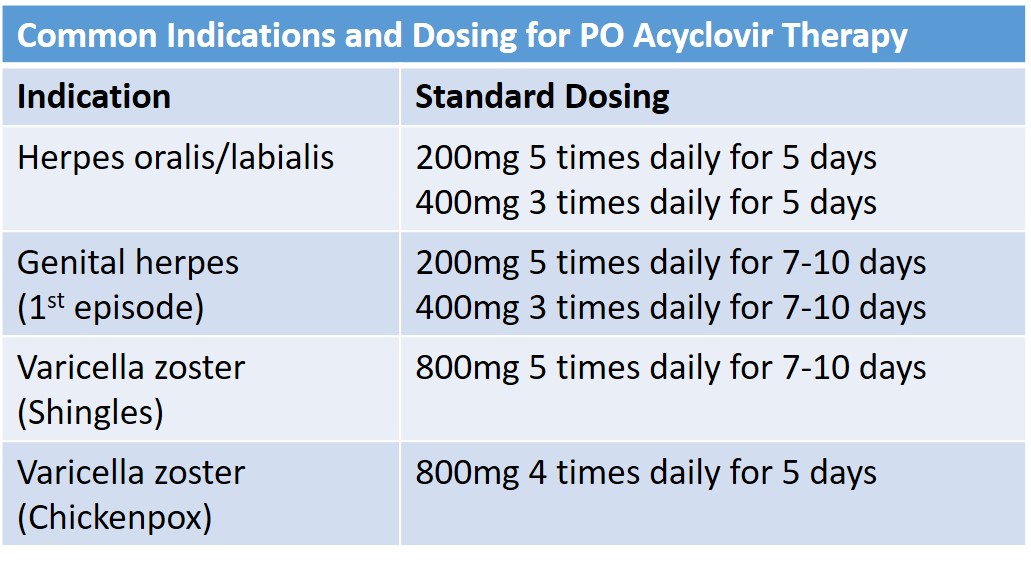
Case Presentation: A 64-year-old woman with end-stage renal disease (ESRD) on peritoneal dialysis (PD) presented with altered mental status. She reported “seeing monsters when I close my eyes,” “bouncing off the walls like I was drunk,” and slurring her speech at home. Her family added that she was highly functional at baseline, lived independently and worked as a caregiver several days a week. Three days prior to presentation, she was diagnosed with herpes labialis and oralis and started on acyclovir 800mg 5 times daily for a 7-day course. She had been too disoriented to perform PD the previous evening. On exam, she was afebrile and hypertensive with SBP 160s-190s. She appeared anxious, disheveled, and was disoriented to time and date but was able to follow commands. She had crusted ulcerations along the border of her lower lip with additional vesicular lesions on her buccal mucosa, hard palate, and tongue. She had no other rash and had a normal neurologic exam and no nuchal rigidity. A CT head was normal and laboratory work-up was unremarkable from her baseline. Lumbar puncture was considered but deferred due to high suspicion for acyclovir toxicity and patient agitation. Her home PD was resumed with nephrology’s guidance. Despite gradual escalation of her PD with increased dwell times, her hallucinations and anxiety persisted. After multiple, interdisciplinary discussions that included the patient and family, the decision was made to defer lumbar puncture and hemodialysis and continue to pursue PD clearance. By hospital day 4, her hallucinations dissipated and she had returned to her baseline mental status, and she was able to be discharged home.
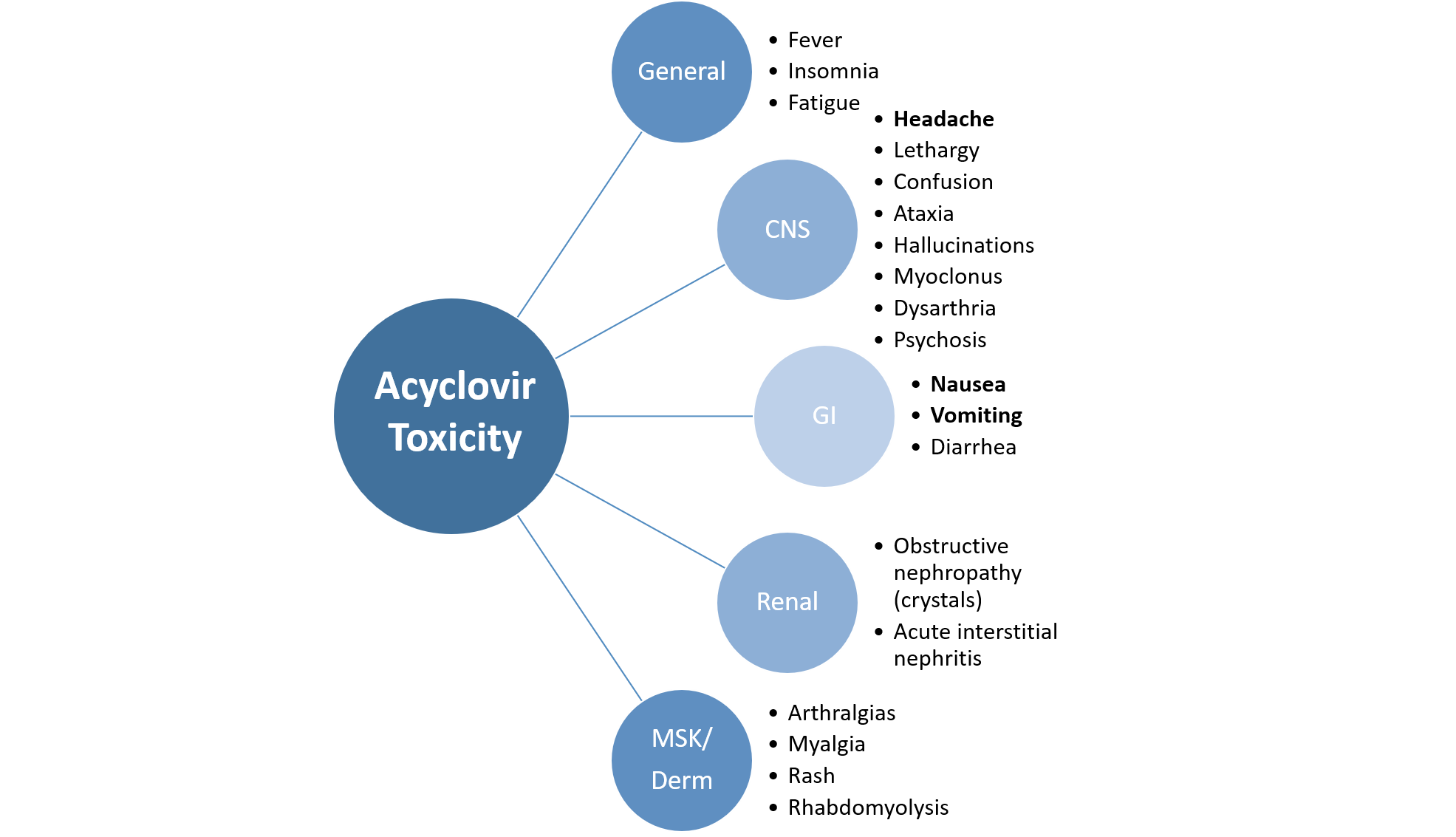
Discussion: Altered mental status in the elderly is a common, yet complex, complaint encountered frequently by hospitalists. The broad differential can inadvertently lead to expensive diagnostic tests and invasive procedures, particularly when there is substantial overlap of CNS infection with drug toxicity symptoms. In this case, the patient’s history of high-dose acyclovir use without renal dose adjustment for peritoneal dialysis, inappropriate dosing for a cutaneous HSV infection, and lack of additional infectious symptoms pointed to acyclovir as the most likely culprit causing her acute encephalopathy. Most case reports involving acyclovir neurotoxicity in patients with ESRD ultimately resolved with initiation of hemodialysis, but for our patient this was not an ideal option given prior fistula complications, altered mental status potentially making a central line insertion higher risk, and family’s strong preference to avoid a hemodialysis catheter.
Conclusions: This case demonstrates the need for increased awareness of medication toxicity in patients on PD, as many case reports have documented acyclovir neurotoxicity even at appropriately adjusted doses. Our patient’s course was prolonged by PD’s inefficiency at clearing acyclovir and the paucity of data to guide dose and duration of PD before more invasive forms of clearance, such as hemodialysis, are indicated. Her full recovery suggests that augmented PD may be a viable option for patients diagnosed with acyclovir neurotoxicity who do not wish to undergo invasive procedures or have relative contraindications to central line placement and are able to remain in a monitored setting.