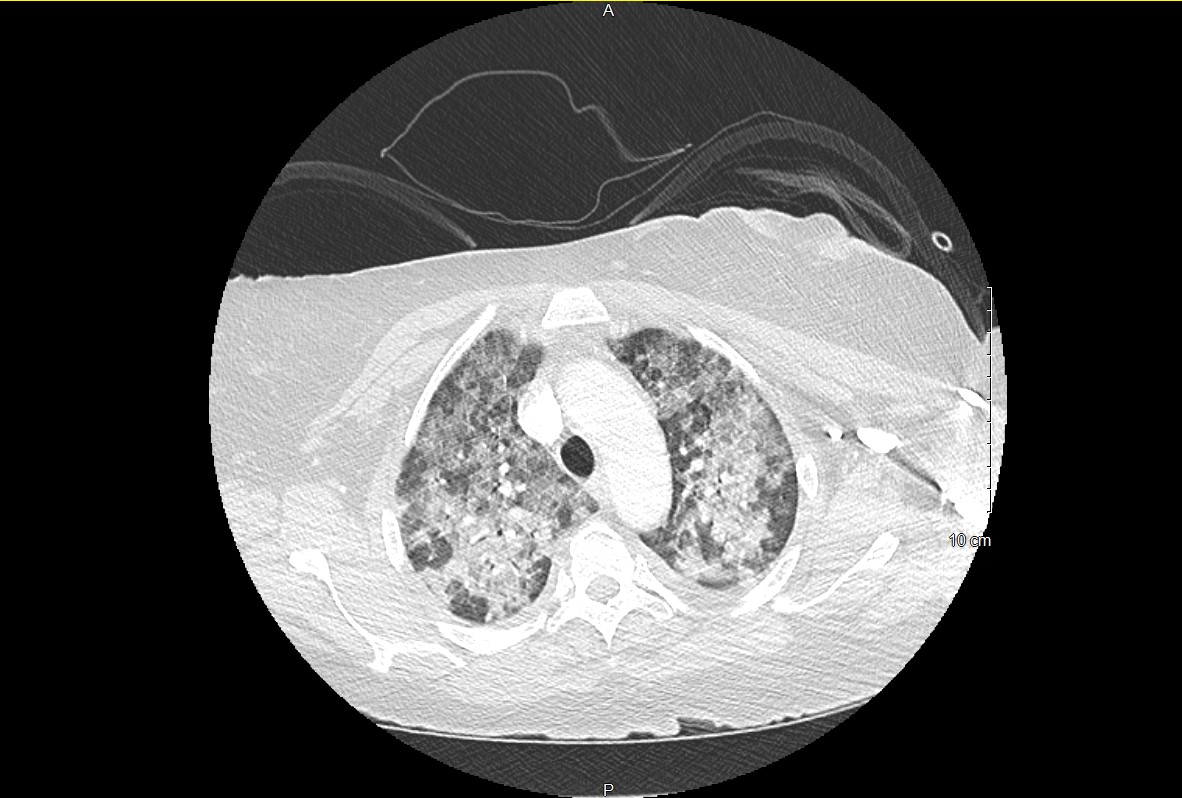
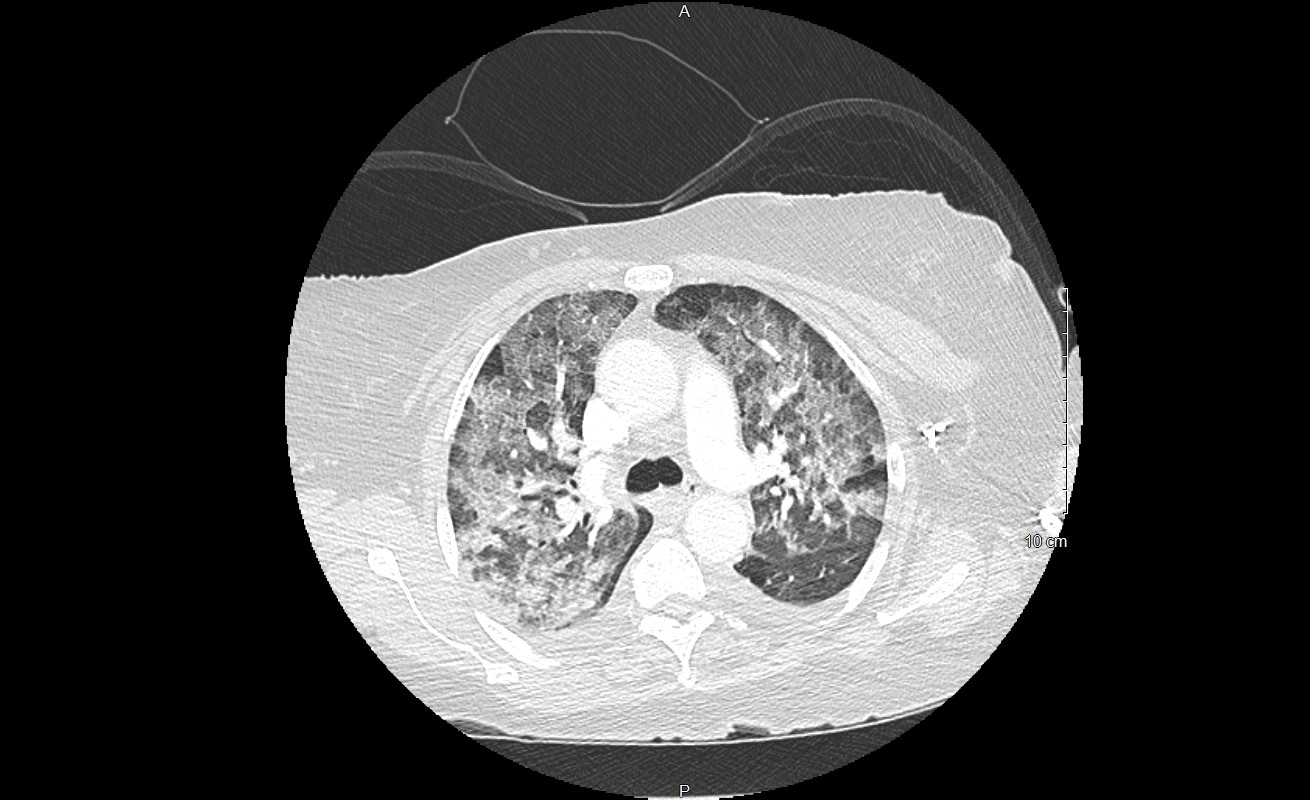
Case Presentation: 63-year-old female with medical history significant for idiopathic thrombocytopenia purpura (ITP), requiring splenectomy in 2013, pulmonary embolism requiring IVC filter placement due to ITP and asthma, presented with acute onset of shortness of breath. Patient had diffuse petechial rash on extremities. She was tachypneic, hypoxic and had rales on examination. Initial evaluation with CBC showed anemia with hemoglobin of 5.4 gm/dl and severe thrombocytopenia with platelets of 3 K/cu mm. CT angiogram of the chest revealed extensive alveolar type airspace opacities throughout both lungs which either represent pulmonary edema or multifocal pneumonia. Patient was admitted to ICU and was empirically started on broad spectrum antibiotics, diuretics and systemic steroids. Patient was transfused blood and platelets, with minimal improvement in platelets. 2 D echocardiogram showed preserved EF. Patient had no neurological symptoms, normal creatinine and no schistocytes on peripheral smear, suggestive of ITP rather than thrombotic thrombocytopenia purpura. She subsequently developed large volume hemoptysis, raising concerns for diffuse alveolar hemorrhage (DAH) in the setting of severe thrombocytopenia. Patient subsequently required noninvasive ventilation due to worsening hypoxemia and increased work of breathing. Platelets remained low despite platelet transfusions, high dose steroids and intravenous immunoglobulin (IVIG) therapy. Patient was started on Romiplostim and Rituximab for refractory ITP. Bronchoalveolar lavage BAL confirmed the diagnosis of DAH. Autoimmune workup including ANA, ANCA, Proteinase 3 antibody, antimyeloperoxidase antibody was negative. Patient underwent bone marrow biopsy which showed hypercellular (80%) marrow with megakaryocyte hyperplasia and erythroid predominant hematopoiesis. Platelet count improved to 67 K. Patient was subsequently weaned off supplemental oxygen.
Discussion: Diffuse alveolar hemorrhage (DAH) is a rare and life-threatening complication of ITP, and prompt initiation of therapy can be lifesaving. DAН is characterized by bleeding into the alveolar spaces of the lungs. DAH should be suspected in patients with hemoptysis, diffuse radiographic infiltrates, anemia and respiratory failure. DΑH is associated with a wide variety of disease processes such as vasculitis, drug induced liver injury, stem cell transplantation, infection, coagulopathy and thrombocytopenia. Flexible broncoscopy with BAL is preferred method of diagnosis of DAH and should be performed promptly to expedite the evaluation. Prompt initiation of therapy is required due to the life-threatening nature of DΑΗ. Corticosteroids and IVIG therapy are the mainstay of treatment for patients with DAH associated with ITP. Alternative treatment strategies including thrombopoetin receptor agonists (TPO RA) and Rituximab should be considered early in refractory cases and in patients with severe and persistent ITP with lethal hemorrhages.
Conclusions: There have been very few reported cases of DAH in association with ITP, which poses significant challenges for clinicians, underscoring the need for increased awareness and prompt clinical management. Identifying the underlying cause is essential to successful treatment. Clues to the underlying cause of DΑH may be identified through a detailed history and physical examination, serologic, hematologic work up, rаԁiοgrарhiс studies, BAL stains and culture, and biopsy of affected tissues.