Background: The Intermediate Care Unit was developed in the 1960s and 70s as a level of care between general medicine (GMU) and intensive care units (ICU) [1]. While all IMU patients could be cared for in an ICU, hospitals have too few ICU beds to accommodate patients who are not critically ill, and higher levels of care often require higher costs. The Society of Critical Care Medicine has established guidelines for admitting patients to an IMU based on severity of illness or need for frequent or complex nursing care [2].
Methods: During a 14-day period, two Hospital Medicine physicians and a patient flow nursing manager retrospectively reviewed each chart by reading provider notes and reviewing objective data for IMU care needs as listed in Table 1. Each patient day was identified as either appropriate or inappropriate for IMU based on these criteria. When the reviewers were unable to identify appropriate IMU criteria, the primary care provider for the patient was contacted by an MD reviewer to discuss the rationale for ongoing IMU level of care. If no appropriate rationale for IMU care was identified, the reviewing physician suggested downgrading the patient to a GMU. The decision of appropriate care level was always decided by the physician primarily responsible for the patient’s hospital care.
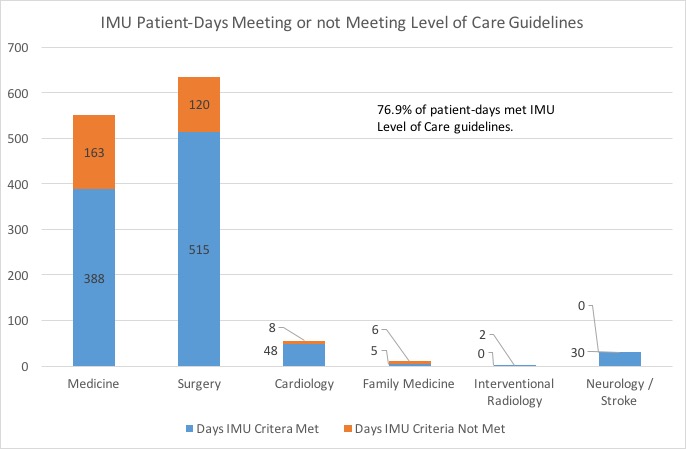
Results: 1053 patient-days were reviewed over the 14 day intervention period, and 365 (34%) of patient-days were identified for which patients at IMU level of care did not meet IMU criteria. For each patient not meeting IMU criteria, the current primary care team was called to ask if these patients could be downgraded to a general medicine ward. Figure 1 shows the number and fraction of patients downgraded by service. The overall downgrade rate to GMU care after intervention was 73.7%. The majority of the patients identified for possible downgrade were on Medicine (n = 127) or Surgical (n = 197) services. The most common reason given for not downgrading patients was concern for risk of clinical deterioration.
Conclusions: Effective clinical quality improvement research can positively impact day-to-day practice of medicine. Efficient patient flow and decrease in healthcare costs are constant challenges to inpatient care. Appropriate use of IMU beds and associated intensive nursing care could both improve costs and patient flow in and out of ICUs and Emergency Departments. This study identified an intervention that could significantly increase the appropriate use of IMU beds. In this study, direct physician review and intervention over a 14-day period revealed that 34% of IMU patient-days did not meet IMU criteria. Physician reviewer intervention led to a 73.7% decrease in inappropriate IMU use. These results could lead to both cost savings and improved inpatient flow. The major limitation of this intervention was the significant time required for daily review and calls by two physicians. Further work is needed to see if other less resource intensive interventions might also improve appropriate IMU use.